
Fortune News | Nov 18,2023
Feb 27 , 2021
By Halima Abate (MD)
Around the world, there are wars taking place within countries that lead to displacement and violence. Ethiopia is no different, unfortunately, with a worrying armed conflict in Tigray Regional State that started in November 2020.
There should be no doubt. Conflict affects all parts of a country, particularly in terms of growth and development, mainly if it is protracted. Moreover, they profoundly impact people that are not active combatants, especially the vulnerable. Wars destroy complex socioeconomic infrastructure and arrangements, including those related to health.
It vividly generates tension between the needs and availability of social protection. It is such areas that are in dire need of humanitarian coverage and access for the vulnerable. It is also the case that these parts are likely to lag behind and get a decreased accessibility to coverage.
During times of armed conflict, countries are generally unable or unwilling to provide adequate health services to their population – in the latter case, it is usually the fear that such services might be abused. In such situations, the public should find the courage in its convictions to denounce attacks on health and health-related infrastructure and lack of access to aid services, whoever might be the culprit.
It is critical to speak out loud and clear that shortages in medical supplies, health personnel and a health workforce could have devastating impacts upon the vulnerable and could only worsen the situation. When citizens cannot access health services due to increased insecurity, or legal and administrative barriers, the health concern will only grow in severity and its long-term consequences. It means the health workforce, nursing homes, pharmacies, community clinics and emergency care services are closed, with little alternative avenues for desperate people with a health emergency.
Due to insecurity and instability, travelling to and from health facilities can be difficult and dangerous. This much is understandable. But creating safe access by both sides of the fighting for such critical services to pass through should not be at all debatable.
The problem, of course, only improves to a degree when there is indeed access to humanitarian and health services. There is a tendency to focus on emergencies, which should be, but there is also an under-prioritisation of sexual, reproductive health or mental issues. Unsustainable, short-term humanitarian interventions do not readily transition to longer-term development work. Health actors are also insufficiently made accountable to affected populations for their performance – chances of suing over medical malpractice are nil – and state-centric health frameworks in countries such as Ethiopia cannot meet the needs of the populace. This is especially true if the nation has a health system stretched by the demands of the Novel Coronavirus (COVID-19) pandemic.
Contemplating our country’s scenario, first and foremost, there should be federal government recognition of the overriding need for public health intervention and unfettered access to aid workers to address the problem. It should result in directing the federal government's machinery in alleviating the health hardships of the populace in vulnerable regions.
Among others, the preparedness for disasters should be rationalised, following international laws and experience, to make it consistent and its constructive impacts long-lasting. There should be the management of pre-impact, impact, and post-impact analysis followed by recovery, rehabilitation and reconstruction. Hence, there should be an implementation of context-specific health policies and interventions where key development actors participate in health clusters and coordinate among themselves. They should facilitate the exchange of comprehensive information with humanitarian health actors, including performance accountability and financial accountability. Nothing less should be expected when it comes to the unfolding situation in the country's north.
PUBLISHED ON
Feb 27,2021 [ VOL
21 , NO
1087]


Fortune News | Nov 18,2023

Radar | Feb 06,2021

Commentaries | Aug 17,2019

Radar | Dec 04,2021

Radar | Jul 24,2023

Featured | Jul 13,2019

Fortune News | Nov 14,2020

Featured | May 18,2019

Radar | Apr 06,2019

Radar | Feb 25,2023

Photo Gallery | 180530 Views | May 06,2019

Photo Gallery | 170724 Views | Apr 26,2019

Photo Gallery | 161800 Views | Oct 06,2021

My Opinion | 137289 Views | Aug 14,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Nov 1 , 2025
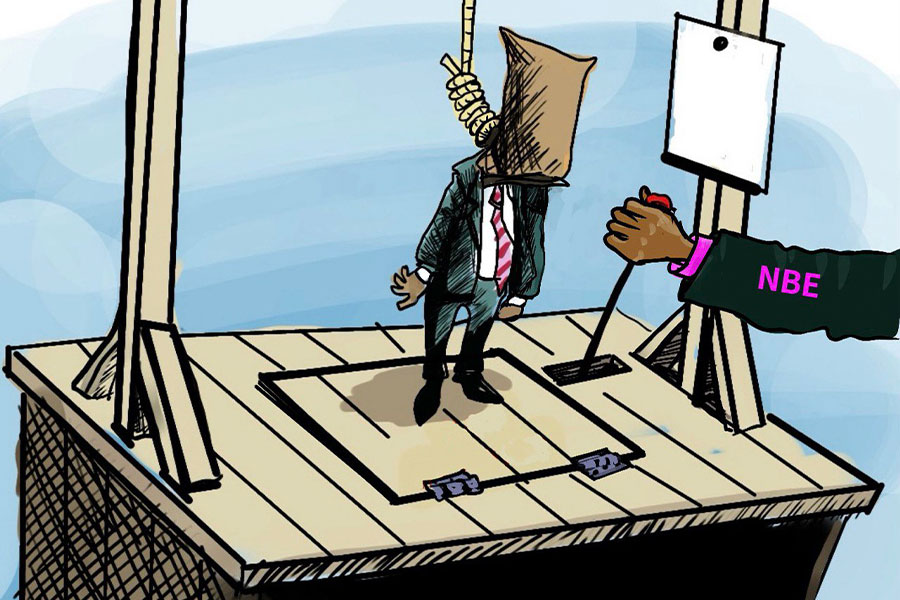
The National Bank of Ethiopia (NBE) issued a statement two weeks ago that appeared to...
Oct 25 , 2025
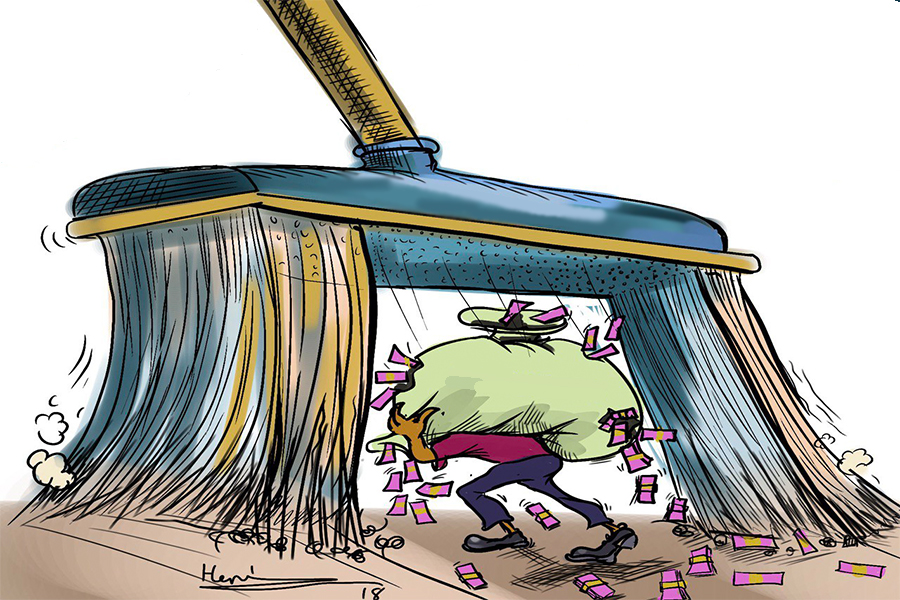
The regulatory machinery is on overdrive. In only two years, no fewer than 35 new pro...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Nov 2 , 2025
The National Bank of Ethiopia (NBE) has scrapped the credit-growth ceiling that had s...

Nov 2 , 2025 . By SURAFEL MULUGETA
The burgeoning data mining industry is struggling with mounting concerns following th...

Nov 2 , 2025 . By YITBAREK GETACHEW
Berhan Bank has chosen a different route in its pursuit of a new headquarters, opting for a transitional building instea...

Nov 2 , 2025 . By BEZAWIT HULUAGER
Nib International Bank S.C. has found itself at the epicentre of a severe governance...