Radar | Oct 23,2018
The Ethiopian Health Insurance Agency (EHIA) will launch novel social health insurance, allowing individuals working in the formal sector to be covered by an affordable health insurance scheme administered by the state.
It is a policy that would enable employees of private entities and public enterprises to lessen out of pocket payments for medical expenses and attain access to healthcare services using a pool of funds contributed in the form of membership fees.
A part of the life insurance lines of business, policyholders of health insurance are very few in Ethiopia. Life insurance constitutes around five percent of the total premiums written by insurance firms, which reached 15 billion Br during the last fiscal year. Insurers have been pleading to implement a mandatory health policy, similar to third-party motor insurance, to buck this trend. The new scheme does not, however, include plans to incorporate the private sector.
The draft directive gives the Agency the sole mandate to collect the funds for the scheme from employees and pay claims to partner healthcare institutions. But for insurers, the new scheme has the potential to turn things around, though only if options for public-private partnerships are put on the table.
"We'd be happy to work with the Agency after reviewing the policies," said Gudina Legesse, CEO of Awash Insurance, which wrote over 330 million Br in life insurance premiums last year, the highest figure among private insurers.
Involving the private sector to assure sustainable social health insurance is crucial for the scheme's success, says Fikru Tsegaye, an executive officer for strategy and development for Ethiopian Reinsurance and an expert in the insurance industry with two decades of experience. The state certifies the health professionals and builds infrastructure, and private insurance firms have the knowledge and skill, according to Fikiru.
"If the implementation is guided by well-designed policies and properly regulated, it will enhance the healthcare ecosystem," said Fikru.
While only those with full employment are eligible for social health insurance, family members will also enjoy similar benefits under the scheme, measures officials of the Agency hope will protect households from financial burdens arising from medical costs. Out-of-pocket spending is high in Ethiopia, accounting for 37pc of the total expenditure in the health sector, according to a 2018 report from the World Bank.
Employers are expected to contribute six percent of the monthly fee, with half covered by employees. The salary contribution of employees depends on their monthly earnings and is voluntary, but the amount determines the scope of benefits they are entitled to. With the collected funds being non-returnable even if employees leave their jobs, the scheme is designed to enable them to get medical treatments ranging from basic checkups to intensive surgical procedures. However, the scheme does not cover work-related injuries.
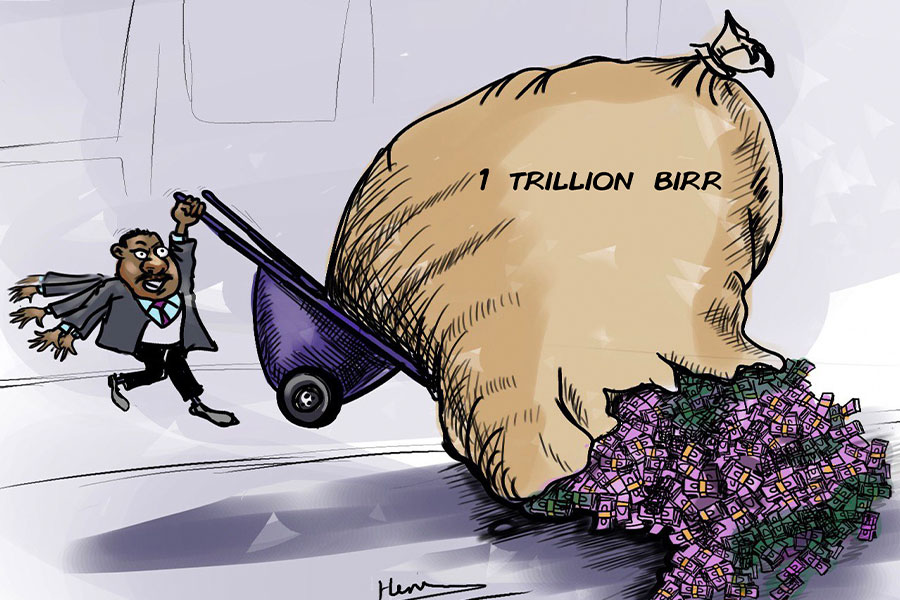
The scheme is also hoped to subsidise the public health costs, which account for six percent of the annual budget that stands at a little over half a trillion Birr this fiscal year.
Launching social health insurance is one of the mandates of the Agency. However, the preparation took time as there was no detailed legal framework to govern the scheme, which will provide citizens employed in the formal economy access to health insurance benefits, according to Halima Abate (MD), director of the Agency. The directive drafted for implementing the scheme aims to improve the accessibility of healthcare services to workers and their families, especially in the case of emergencies, said Halima.
Following the passing of the directive, the scheme will be implemented in two rounds, Halima disclosed.
Members of the civil service and pensioners will be the first beneficiaries, followed by those employed by state enterprises, the private sector and non-governmental organisations.
Absera Bekele is a public servant with a monthly income of 5,300 Br. She welcomes the introduction of the scheme, despite having some reservations about the premiums expected from her.
"The premium has to be considerate of a living standard," she said.
Established in 2010 as a federal agency with 24 branch offices, the Agency has been operating with a community-based health insurance (CBHI) scheme over the last decade, enabling access to healthcare services for over eight million households, most of which reside in rural areas. The modality covers communities engaged in the informal sectors of the economy, particularly in agriculture, in close to 900 woredas of the Amhara, Oromia, Tigray and Southern regional states, as well as Addis Abeba.
The Agency has collected 2.2 billion Br and signed agreements with over 3,000 health centres in these states under the scheme with a benefits package covering all outpatient and inpatient services at health centres except dental, ophthalmology, and cosmetic procedures.
According to Dinka Erena, coordinator of CBHI in the Oromia Health Bureau, the demand for the service is increasing. The number of beneficiaries increased by almost two-thirds last year. Around 4.4 million people are signed up in the Regional State, where over 8,500 health facilities operate. The Bureau has so far collected over one billion Birr to fund the scheme.
Most of this money comes from the beneficiaries themselves, mostly farmers, who were charged a yearly premium of 250 Br in rural areas and 360 Br in urban settings. This has now been adjusted to match rising healthcare costs, and they will be expected to pay 410 Br and 510 Br, respectively.
PUBLISHED ON
Aug 21,2021 [ VOL
22 , NO
1112]
Radar | Oct 23,2018
Radar |
Sunday with Eden | Aug 08,2020

My Opinion | Feb 16,2019

Fortune News | Jul 21,2024

Radar | Nov 09,2024

News Analysis | May 06,2023

Life Matters | Sep 07,2019

Radar | Jan 18,2020

Radar | Mar 02,2019

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Jul 5 , 2025
Six years ago, Ethiopia was the darling of international liberal commentators. A year...

Jun 28 , 2025
Meseret Damtie, the assertive auditor general, has never been shy about naming names...
Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...

Jun 14 , 2025
Yet again, the Horn of Africa is bracing for trouble. A region already frayed by wars...