
Oct 21 , 2023
By Lennie Bazira , Prossy Muyingo
The global commitment to "health for all" is incomplete without addressing the plight of community health workers. Investing in this mostly women workforce is not just about investing in health but in justice, equity, and a brighter future for all, argue Lennie Bazira, a policy director of the Community Health Impact Coalition, and Prossy Muyingo, a community health worker in Uganda, in this commentary provided by Project Syndicate (PS).
At least six million women worldwide provide unpaid or grossly underpaid labour in community health centres, often in low- and middle-income countries (LMICs). Many work as community health workers(CHWs). But, though this is a skilled job that should be salaried, only 34 countries offer CHWs accreditation, training, and salaries, leaving the majority exploited and, therefore, less effective for their patients. This must change if we are serious about making "health for all" a global priority.
CHWs are crucial to strengthening health systems at the national level: they have been proven to improve maternal- and child health services, expand access to family planning, and support prevention and care for both non-communicable and infectious diseases. Deploying CHWs who consistently provide 30 lifesaving health services in countries with the highest disease burden would save as many as 6.9 million lives annually and reduce child mortality by almost half.
The COVID-19 pandemic demonstrated how resilient community health programs can provide essential services even in the face of great adversity.
However, such programs will reach their full potential only with service design that adheres to evidence-based best practices. That means treating CHWs as professionals who require training, fair pay, and safe working conditions. When used as a stopgap solution or a source of cheap labour, CHWs are less effective than their well-resourced counterparts.
In Africa, up to 85pc of CHWs are unpaid; and, worldwide, CHWs' essential medicines are out of stock one-third of the time. CHWs have stepped up to fill the gap in Uganda, our home country, with a shortage of healthcare workers. Though these workers provide vital services to their communities, performing many of the same tasks as their salaried supervisors, they often receive little or no pay.
Why are CHWs, often women of colour, expected to work and save lives without recognition or remuneration?
It is clear that this is also a gender-rights issue. Patriarchal norms and power dynamics condition women to accept no or low wages for what should be paid work. For example, women from low-income households and with low levels of education often view this type of unpaid work as an opportunity that might lead to paid work or an asset like a mobile phone or bicycle. Unpaid work in healthcare can also bring women social recognition. In many contexts, it is seen as honourable work that families will approve of for a woman.
As a result, CHWs tend to juggle these positions with piecemeal paid jobs and family responsibilities.
These women face an unenviable dilemma: If they give up their work as CHWs to find full-time employment that can support them, who will provide much-needed healthcare for their communities?
Backed into a corner by systemic inequalities and traditional gender roles, they often continue to overextend themselves, sacrificing stability, economic security, career progression, and well-being.
To redress this entrenched social and economic injustice, professional CHWs must become the norm, not the exception. At minimum, CHWs must be accredited to ensure that certain standards are met; paid a competitive wage; continuously trained and supported by a dedicated supervisor; and integrated into health systems, including primary healthcare facilities and broader monitoring and evaluation systems. That way, they can be proactive in surveillance and see patients without point-of-care user fees.
In short, community health workers must be salaried, skilled, supervised, and supplied.
After years of marginalisation and isolation, they are now organising and establishing in-country networks, mainly using digital technology, to achieve these goals. More than 5,000 CHWs and aligned health organisations across 40 countries have come together via the Community Health Impact Coalition to translate shared research and advocacy work into policy change at the national level. Our shared mission is to ensure that all law and middle-income countries adopt policies for professional CHWs.
The global community must decide whether it will fairly compensate those who, for decades, have propped up health systems in these countries, or continue to exploit a predominantly female workforce. The moral choice is clear. Countries that professionalise CHWs and integrate them into a robust health infrastructure will be in the best position to make progress toward "health for all" – including the women delivering the bulk of the care.
PUBLISHED ON
Oct 21,2023 [ VOL
24 , NO
1225]

Commentaries | Jun 08,2024

Agenda | Jun 17,2023
Sunday with Eden | Mar 23,2024

Radar | Nov 26,2022

Fortune News | Mar 13,2021

Viewpoints | Nov 05,2022

Radar | Nov 09,2024

Radar | Mar 26,2022
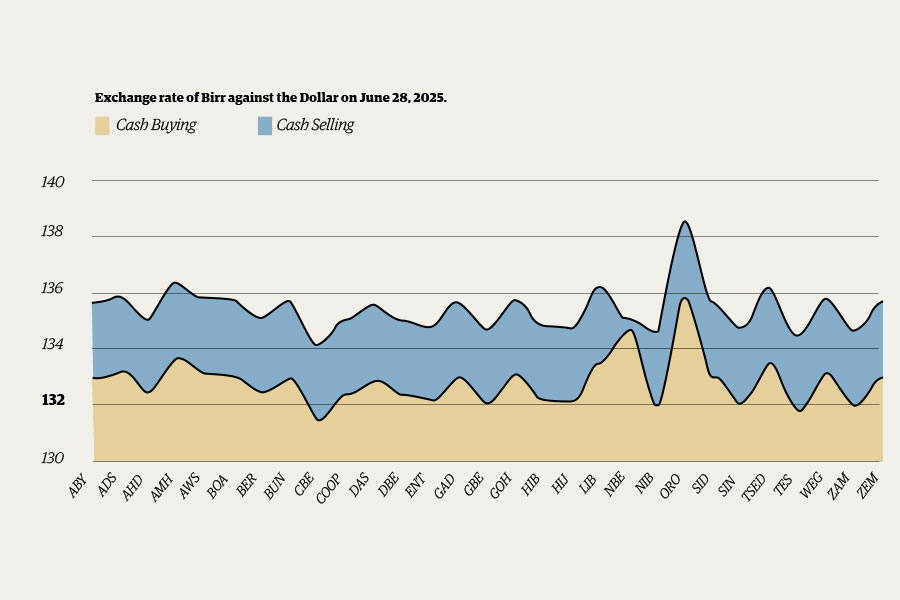
Money Market Watch | Jul 06,2025

Sunday with Eden | Jan 12,2019

My Opinion | 132151 Views | Aug 14,2021

My Opinion | 128561 Views | Aug 21,2021

My Opinion | 126482 Views | Sep 10,2021

My Opinion | 124091 Views | Aug 07,2021





Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Jul 12 , 2025
Political leaders and their policy advisors often promise great leaps forward, yet th...

Jul 5 , 2025
Six years ago, Ethiopia was the darling of international liberal commentators. A year...

Jun 28 , 2025
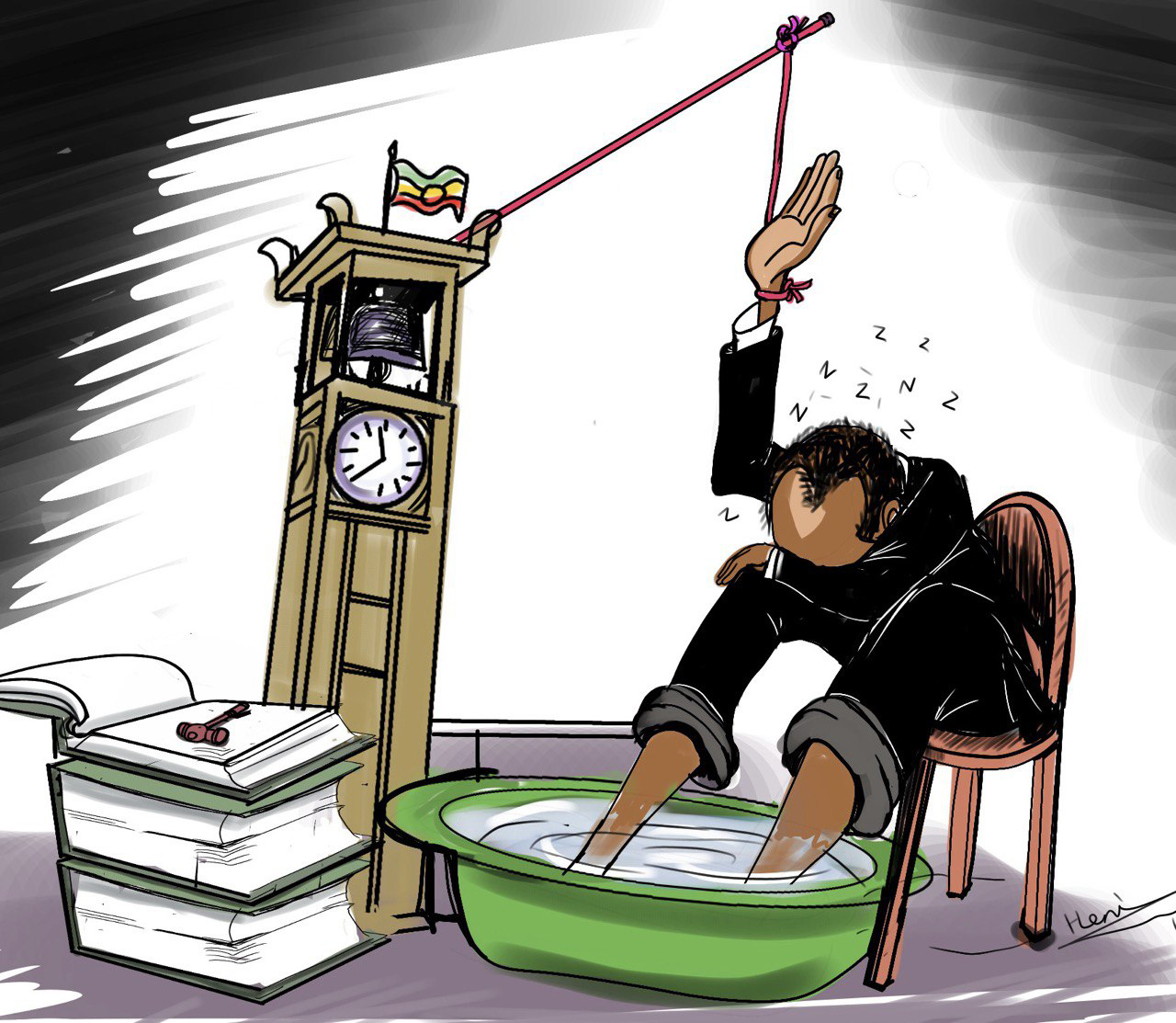
Meseret Damtie, the assertive auditor general, has never been shy about naming names...

Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...

Jul 13 , 2025 . By YITBAREK GETACHEW
The Addis Abeba City Revenue Bureau has introduced a new directive set to reshape how...

Jul 13 , 2025 . By BEZAWIT HULUAGER
Addis Abeba has approved a record 350 billion Br budget for the 2025/26 fiscal year,...

Jul 13 , 2025 . By RUTH BERHANU
The Addis Abeba Revenue Bureau has scrapped a value-added tax (VAT) on unprocessed ve...

Jul 13 , 2025 . By NAHOM AYELE
Federal lawmakers have finally brought closure to a protracted and contentious tax de...