
Commentaries | Jun 22,2019
Oct 14 , 2023
By Selome Getachew
Every year, the world celebrates World Mental Health Day on 10 October. The theme for this year, set by the World Foundation of Mental Health, was ‘Mental health is a universal human right’. It is a moment marked to raise mental health awareness and drive positive change for patients and victims.
Individuals with mental health issues are known to be reluctant to seek professional care due to fear of being labelled as “insane”, mistrust of the system, and a lack of faith in medical personnel.
In Addis Abeba, encountering mentally affected individuals, unconsciously exposing themselves to the world, is resurging. Some even resort to violent behaviours, blocking roads, and hurling stones at cars, and unsuspecting passersby.
Behind closed doors, mental health issues in Ethiopia have been swept under society’s rug, burdened by stigma and met with ignorance, causing countless individuals to suffer in isolation without vital support. The combination of substance abuse, particularly khat, and the fast-paced, stress-ridden lifestyle prevalent in the country further exacerbate the likelihood of experiencing depression or anxiety.
The World Health Organization’s (WHO) unique initiative for mental health reveals that almost four out of five people globally with mental illness, including substance abuse and neurological disorders, do not receive the necessary quality and affordable mental healthcare.
Ethiopia finds itself on the precipice of a mental health crisis. Sadly, there has been limited data on the potential mental health consequences of the war in Ethiopia.
A study conducted by the Borgen Project reveals that despite an estimated 15pc of Ethiopians, from a population exceeding 100 million, suffer from mental illness and substance abuse disorders. Fewer than 100 psychiatrists serve in less than 20 hospitals equipped to address this urgent need.
Experts working for the WHO estimate the populations in the war-affected regions of Tigray, Afar and Amhara have close to 30,000 individuals facing severe mental health disorders requiring immediate intervention. Of these, over 90pc are children and women.
The rise in mental disorders can be attributed to urbanisation, rapid social changes, poverty, and increasing stressors.
Cultural beliefs and misconceptions cloud the Ethiopian perspective on mental health. Many still attribute mental illnesses to supernatural forces or malevolent spirits, stigmatising and marginalising those affected. This skewed perception not only stands in the way of compassion within society but also perpetuates a vicious cycle of isolation for those struggling with mental health issues.
Milder forms of mental disorders often go unrecognised, considered instead as mere acts of “bad behaviour.” Severe cases are dismissed as untreatable conditions. Phrases often thrown around, such as “insane” or “crazy” further deepen the wounds, undermining progress towards a society that embraces and supports individuals with mental illness.
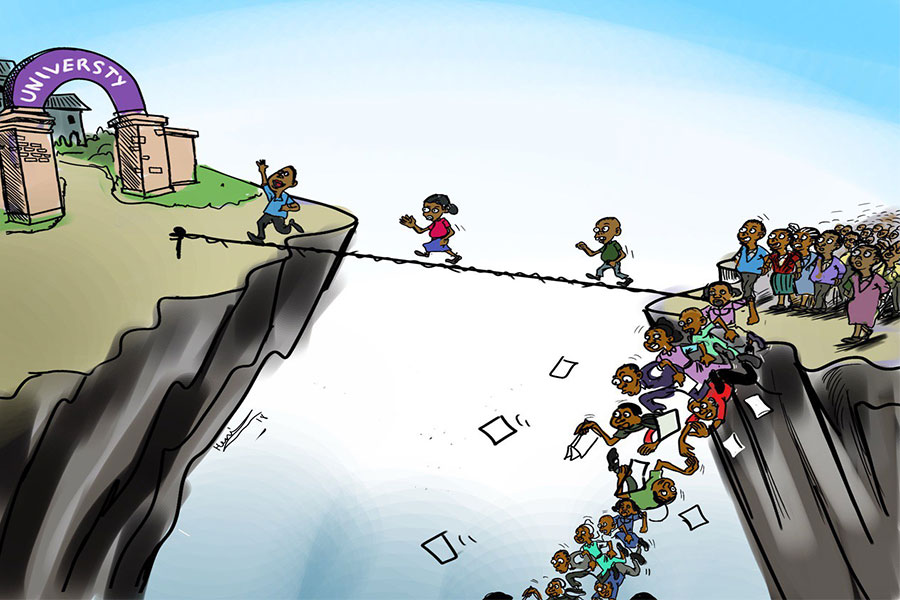
Individuals with mental disorders are left without access to effective care, and labelled as “odd”, “unfriendly”, or “annoying”. This dire situation is particularly evident among university students, whose academic pursuits are often derailed by unrecognised mental health issues. Neglecting milder cases can lead to critical conditions and perpetuate lifelong hardships, as illustrated by the story of an exceptional student at Addis Abeba University (AAU) who fell victim to delusional disorder.
Unknown to her peers, this student was convinced that every person she encountered and signs she saw contained secret messages addressed to her. Delusional disorder, a type of psychotic disorder, caused her to lose touch with reality, consequently experiencing deep distress and impairment in her daily functioning. Her desperate attempts to interpret these false messages led her to follow strangers, further isolating her from those around her.
A family member - a medical professional - recognised her condition and facilitated timely treatment. However, her journey is one of thousands, representing the countless university students, housewives, and young men and women who remain misunderstood and abandoned, sliding further into a relentless abyss.
When individuals tend to isolate themselves because of depression, they are often unfairly deemed unsociable. Individuals with attention deficit disorder are often misunderstood, with their symptoms mistakenly attributed to laziness or lack of intelligence. Those suffering from delusional disorder may have their lives disrupted by preoccupying delusions, yet friends and family frequently dismiss their cases as harmful or irritating.
Such dismissive attitudes can lead individuals to develop chronic mental disorders, and, in the worst cases, result in suicidal tendencies.
Recognising and confronting the less severe manifestations of mental disorders is crucial. A fundamental shift in societal judgment is imperative. Those struggling with mental health issues should not be ostracised, but rather be given the support needed to reintegrate into society.
Treating all patients in the same facility may alienate those with milder conditions, who may feel unfairly categorised alongside individuals with more severe disorders. While mental health clinics play a pivotal role in providing services such as medication management, psychotherapy, and counselling, the number of patients seeking help often makes individualised counselling a luxury.
Differentiating between severe and mild cases is crucial in providing appropriate care centres. Counselling and consistent follow-up are essential in maintaining the delicate balance between medication and psychological support for individuals in the early stages of mental illness. But, this is hardly found in the psychiatry clinics in service.
One of the oldest and well-known such centres is St. Emanuel Hospital, serving inpatients and outpatients, embracing not only those battling mental afflictions but also those navigating through other medical tribulations. Of the mere 259 beds, 11 are reserved for patients requiring privacy, and 23 stand vigilant as emergency beds, ready to rush to the aid of those in distress.
Each month, no less than 10,320 patients find solace within these walls, yearning to reclaim a life unfettered by mental anguish. Despite its ceaseless commitment, the Hospital succumbs to its capacity limitations. Alas, the scarcity of beds compels patients to wait up to half a year before finding admission.
The integration of mental healthcare into primary healthcare remains insufficient. As devoted members of the global development community, we are obligated to do more, offer more, meet the dire needs of those afflicted by mental health disorders, and provide aid to those most heavily impacted. Our focus should be prevention, identifying and intervening before concerns spiral out of control.
The significance of mental health advocacy cannot be understated; it plays an essential role in nurturing the well-being of both individuals and communities. We must cultivate societal awareness about the early stages of mental health disorders.
PUBLISHED ON
Oct 14,2023 [ VOL
24 , NO
1224]


Commentaries | Jun 22,2019

Fineline | Jan 15,2020

Advertorials | Jan 02,2020

Fortune News | Jun 17,2023

Fortune News | Jul 03,2024

In-Picture | Apr 19,2025

Life Matters | May 04,2019

Life Matters | Mar 09,2019

My Opinion | Sep 28,2024

Agenda | Nov 20,2021

Photo Gallery | 176415 Views | May 06,2019

Photo Gallery | 166629 Views | Apr 26,2019

Photo Gallery | 157139 Views | Oct 06,2021

My Opinion | 136908 Views | Aug 14,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
Four years into an experiment with “shock therapy” in education, the national moo...
Oct 18 , 2025 . By NAHOM AYELE
In a sweeping reform that upends nearly a decade of uniform health insurance contribu...

A bill that could transform the nutritional state sits in a limbo, even as the countr...

Oct 18 , 2025 . By SURAFEL MULUGETA
A long-planned directive to curb carbon emissions from fossil-fuel-powered vehicles h...

Oct 18 , 2025 . By BEZAWIT HULUAGER
Transaction advisors working with companies that hold over a quarter of a billion Bir...