
Life Matters | Sep 08,2024
Nov 23 , 2024
By Glenda Gray
Drug development steered by profitability over public health needs has led to the shortchanging of infants in poorer countries. Even when clinicians can access first-line antibiotics, drug-resistant infections often force them to shift to less effective, last-resort options. In this commentary provided by Project Syndicate (PS), Glenda Gray, board chairwoman of the Global Antibiotic Research & Development Partnership, argued children under five make up one in five deaths from drug-resistant infections, with 99.7pc living in low- and middle-income countries.
Over the last half-century, the number of children who die before reaching the age of five has fallen dramatically, from around 20 million in 1960 to 4.9 million in 2022, mainly owing to the expanded programme on immunisation (EPI). Established by the World Health Organization (WHO) in 1974, the programme has been extraordinarily successful in providing the youngest people with access to vaccines, saving more than 150 million lives.
But while such progress is worthy of celebration, much work still exists. Newborns comprise half of all deaths in children under five each year, many of which are caused by infection.
Progress on reducing neonatal mortality has historically been much slower than for children under five. It has begun to stall in recent decades, despite reductions in mother-to-child transmission of HIV, syphilis, and hepatitis. That is because many of these deaths are caused by treatable – but untreated – bacterial infections. To reverse this trend, the international community should ensure that all children – especially in the African countries where most of these deaths occur – can access antibiotics, much like the EPI has done for vaccines.
Infants are particularly susceptible to infections in the first 28 days of life. As a paediatrician, I saw this firsthand when I was younger, working in the neonatal ICU at the Chris Hani Baragwanath Hospital in Soweto. It is possible to ward off some kinds through infection prevention and control; access to water, sanitation, and hygiene; and vaccines. But for those that cannot be prevented, antibiotics are needed to avert further complications, such as sepsis, which affects up to three million newborns a year.
Unfortunately, most African countries lack access to existing and new antibiotics, putting already vulnerable babies at a much higher risk of dying from treatable infections. Shortages of generic versions can be attributed mainly to the steady exit of pharmaceutical companies from the antibiotic market in recent decades, owing to low returns. Similarly, new antibiotics are often sold in only the wealthiest countries or priced out of reach for most African governments and citizens.
For example, less than half of the new antibiotics approved between 1999 and 2014 were registered in more than 10 countries. Worse, only four of the 40 new antibiotics approved since 2000 are labelled for pediatric use. When drug development is driven primarily by profitability rather than public health needs, infants in poorer countries—one of the world's most vulnerable populations—get the short end of the stick.
If clinicians cannot access the right first-line antibiotics or use them because of drug-resistant infection, they often turn to those that are specialised or kept in reserve as a last resort. These substitutes can be less effective, and reliance on them increases the risk of drug resistance developing, making infections more difficult to treat in the long term (although African countries are often priced out of these last-resort antibiotics, too).
As a result, children under five account for one in five deaths caused by drug-resistant infections, with 99.7pc of them living in low- and middle-income countries. At the same time, the failure to treat these infections in newborns is fueling the rise and spread of antimicrobial resistance (AMR), which is already associated with 4.7 million deaths annually.
No country can tackle this problem alone. Ensuring that all infants are protected from infection requires an EPI-scale global initiative to help developing countries build their capacity and surveillance, identify the necessary antibiotics, and bolster their health systems. Equally important, we should dramatically increase the availability of existing antibiotics and spur the development of new ones that are safe and effective for children. Both imperatives require prioritising public health over profit.
The United Nations High-Level Meeting on Antimicrobial Resistance recently produced a political declaration committing countries to reducing global AMR-associated deaths by 10pc a year until 2030. Donor governments can begin doing this – and saving the lives of newborns – by supporting organisations like the Global Antibiotic Research & Development Partnership, which is working to improve access to and encourage the development of antibiotics.
The WHO's Pediatric Drug Optimisation exercises have made a shortlist of antibiotics that should be prioritised above all others for pediatric use. But, stakeholders, including the WHO, regulatory agencies, the pharmaceutical industry, non-profit developers, and pediatric experts, should collaborate to shepherd such treatments through development and approval. Preventing infant deaths from treatable infections would go a long way toward stopping the spread of AMR and safeguarding our future.
PUBLISHED ON
Nov 23,2024 [ VOL
25 , NO
1282]


Life Matters | Sep 08,2024

Commentaries | Mar 23,2024

Commentaries | Apr 28,2024

Covid-19 | Feb 20,2021

Commentaries | Jan 07,2024

View From Arada | Dec 17,2022

Editorial | Dec 25,2021

Commentaries | Apr 26,2019

Commentaries | May 04,2019

Commentaries | Dec 07,2019

My Opinion | 131548 Views | Aug 14,2021

My Opinion | 127903 Views | Aug 21,2021

My Opinion | 125879 Views | Sep 10,2021

My Opinion | 123510 Views | Aug 07,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Jun 28 , 2025
Meseret Damtie, the assertive auditor general, has never been shy about naming names...

Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...

Jun 14 , 2025
Yet again, the Horn of Africa is bracing for trouble. A region already frayed by wars...
Jun 7 , 2025
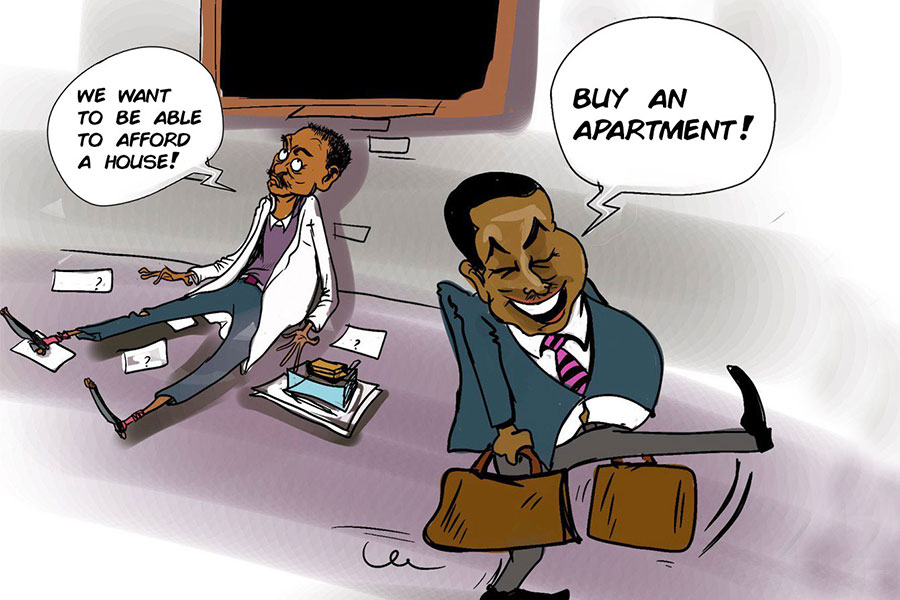
Few promises shine brighter in Addis Abeba than the pledge of a roof for every family...

Jun 29 , 2025
Addis Abeba's first rains have coincided with a sweeping rise in private school tuition, prompting the city's education...

Jun 29 , 2025 . By BEZAWIT HULUAGER
Central Bank Governor Mamo Mihretu claimed a bold reconfiguration of monetary policy...

Jun 29 , 2025 . By BEZAWIT HULUAGER
The federal government is betting on a sweeping overhaul of the driver licensing regi...

Jun 29 , 2025 . By NAHOM AYELE
Gadaa Bank has listed 1.2 million shares on the Ethiopian Securities Exchange (ESX),...