
Radar | Oct 24,2020
A sharp and deafening noise exhales from an oxygen production centre in the Saris neighbourhood, Nefas Silk District. Two sets of enormous machines operate at full capacity; they are so overpowering that sounds nearby are muffled.
It was a scene in sharp contrast to what the area was like about two months ago when it was filled with the desperate pleas from loved ones of at-home patients, begging to get oxygen cylinders refilled. Back then, the team at Gast Solar Plc's plant was overwhelmed by the sheer enormity of oxygen demand from hospitals as well as individual patients.
“Everyone was desperate, asking for oxygen,” said Solomon Be`ededmariam, general manager of Gast.
Solomon has not seen such a huge demand in over a decade when the plant has been in operation, although he observed it growing steadily even before the pandemic hit last year.
The plant is one of three dozen active oxygen production facilities across the country, assets that now determine the life and death of so many since the outbreak of COVID-19 in March 2020. Gast Solar has thus been compelled to work 24-hour shifts to quadruple its production to 160 litres of oxygen an hour. Around 1,200 cylinders need to be refilled a day at this plant, which uses the cryogenic distillation process, extracting oxygen from air by liquefying at shallow temperatures. It meets, however, one-third of the country's current supply.
Chora is the oldest and by far the largest oxygen plant in Addis Abeba. In late March this year, the city lost this medical oxygen supplier while an average of around 2,500 people tested positive for the virus daily and almost half of this number were under intensive care units. A machine broke down at Chora in the midst of the worst days of the pandemic so far. It was a terrifying moment for the operators and those on the frontlines fighting COVID-19, including Solomon, as a critical shortage of life-saving oxygen hit the city.
Frie Admasu recalled this moment of desperation when her mother was sick, contracting the virus.
"I almost lost her," she said.
Frie had to wait for over two days until she found oxygen at the COVID-19 field hospital at Bole Bulbula, where she had stayed for 10 days.
"Imagine the feeling," she recalled. "Your mother is struggling to breathe due to severe pneumonia from COVID-19, while you cannot get oxygen for her nor cover the cost for the same service at a private hospital."
Running around to more than five hospitals and the COVID-19 centre at Millennium Hall, it was only through the help of a friend working at the Bole Bulbula centre that Frie finally succeeded in finding help for her mother. Treatment centres across the city were overwhelmed by the inflow of patients, and the situation was so desperate that the Millennium Hall, converted to one of the biggest COVID-19 treatment centres in Addis Abeba last year and hosting more than 140 patients, had to limit the flow of oxygen allocated to patients.
Intensive care unit at Millennium Hall medical centre treating COVID-19 critical patients.
What ensued at the time was chaos as an already-existing supply gap was worsened by the insurmountable demand caused by a sharply increased number of COVID-19 patients under critical conditions.
Before the pandemic hit, the demand and supply for oxygen were not followed up in a coordinated manner, according to Amanuel Lulu (MD), in charge of oxygen supplies at the national COVID-19 taskforce case management team. It was difficult to identify the demand back then.
"Even at this time last year, we weren't discussing oxygen," said Mikiyas Teferi (MD), head of the national task force.
Things seem to have improved since, indeed, with government-backed efforts to increase supply, seemingly taking the load off hospitals and treatment centres.
There has always been a walloping gap between oxygen cylinders production at the few plants and the demand by hospitals and centres. Of the 315 health centres surveyed by the Clinton Initiative in 2016, only two percent were found capable of providing oxygen. In hospitals, the figure was found to be two-thirds. Several studies conducted on the availability of oxygen and oxygen delivery equipment have corroborated the findings from the Clinton Health Initiative. They mostly highlight the dearth of oxygen supply that has been a contributor to child and maternal mortality.
Oxygen supplies are essential in combating newborn fatalities as a third of babies with pneumonia need oxygen for proper treatment.
This was among the primary driving factors that led to the design and implementation of a “national scale-up of oxygen management” roadmap. Adopted five years ago in collaboration with the Ministry of Health, the road map targeted six key areas, including rolling out an oxygen supply and logistics chain; establishing a mechanism for the maintenance of oxygen equipment; capacity building of health care workers in oxygen provision; and increasing sustainable funding for oxygen procurement.
Of all the plans set out in the roadmap, perhaps the most ambitious was building oxygen plants in 13 public health centres by 2020, which seems to have been achieved, although the production capacity of these centres still needs to grow. What is available now is a far cry from the one billion cubic metres of oxygen production a month the authorities had hoped they would reach by last year, thus showing a long way to go in addressing oxygen supply gaps.
The health centres have not made the noticeable progress over the past five years they were hoped to, according to Habtamu Seyoum, senior programme manager at the Clinton Health Initiative.
Under the stewardship of Lia Tadesse (MD), the Ministry of Health is trying to take a series of measures targeting to fix the broken distribution system. The Ministry pushed four plants supplying oxygen for industrial purposes to supply the medical oxygen demand fully.
With a combined capacity to fill 1,500 cylinders a day, these four plants have helped take the pressure off the current supply chain near to crumble on the weight of ballooning demand.
Authorities at the Ministry have also targeted the restructuring of the supply chain. Previously, hospitals queued up at whatever production centre they found convenient, causing a mismatch between the demand on their end and supply at the plants. The Ministry now tells a health facility or hospital to relieve its oxygen cylinders from a designated supplier.
One of the beneficiaries of this scheme is the Black Lion Hospital, the largest health facility in the country with 1,000 beds.
Much like many other public health centres, the Hospital had to endure the burden of sustaining its services under a severe shortage after its sole supplier, Chora Gas Plant, stopped production. Such a large facility serving as a referral hospital for the whole country had to survive with a supply of just 20 to 30 cylinders a day, significantly less than its usual demand of 150 cylinders.
Yirgu Gebrehiwot (MD), director of clinical services at the Black Lion Hospital, recalls the many nights his medical team was put under a lot of stress, spending intense moments filled with anxiety and disagreements. The medical team had to shift patients with less drastic needs to oxygen concentrators.
With the new scheme, Black Lion is now sourcing its oxygen from three suppliers.
"What could have potentially been a disaster was averted," Yirgu told Fortune, a sense of relief evident in his tone.
The situation has been no different with the private medical centres, especially those delivering COVID-19 treatment.
The American Medical Centre (AMC), a private health centre founded in 2012, has had little to no problems sourcing oxygen in the pre-pandemic era. Designating ward for 10 COVID-19 patients beginning December last year, it started to have issues in the past few months; the Centre's stock run out in two days.
Working in the oxygen supply chain area for the past six years, Habtamu observed the pandemic brought a curse for the health service provision. The diversion of health service provisions to COVID-19 has strained other treatments, not just in Ethiopia but also around the world. Treatments such as surgical operations and those suffering from things such a heart disease are feeling the burn.
"Elective surgery might be facing cancellation, or people are wasting their time looking for oxygen," said Habtamu.
But the blessing could be that it forced the authorities to look closer into an area that has been neglected for far too long, the production and supply chain of medical oxygen.
They are in the frantic mood to rehabilitate existing oxygen plants, restart centres that were left idle, and set up new ones in treatment centres. Oxygen plants in Ambo, Dilla and Jigjiga have gone operational, while Yekatit 12 and St. Peter's public hospitals are lined up to get their respective plants.
Chora Gas Plant is expected to resume production in a few days, Mikias disclosed to Fortune. In addition, the Ministry has set up safety stocks at Millennium Hall and Menelik Hospital for emergency situations. The stock at the Millennium Hall treatment centre holds 1,000 cylinders.
Oxygen cylinders are imported primarily from China. Gast, for instance, owns about 3,000 cylinders, but customers with their own cylinders can also visit the plant for a refill. The prices of cylinders vary depending on sizes, however. Standard costs hover around 6,000 Br, although, during the pre-COVID period, the same equipment with an average capacity of six litres was sold between 3,500 Br and 4,000 Br.
Another loophole adding to a surge in the cost of producing oxygen is regional disparity, whereby certain areas with no oxygen plants have been suffering. Areas like Gambella and Benishangul-Gumuz regional states have had severe shortages. The Ministry is attempting to fill the gap by helping the areas source oxygen from Bishoftu Hospital. Gast has taken on the responsibility of providing technical support to other plants, so far, has helped set up the oxygen plants in Ambo and Dilla.
Supply shortages in remote areas and peripheral regions are indeed an issue that needs to be addressed with its own approach in the next roadmap, according to Habtamu.
Setting up an oxygen plant can cost up to 10 million Br, with procurement of the machines taking up the majority of the cost. But for private plants, their investment could be recouped in less than a year, according to Amanuel.
According to Solomon, the general manager, oxygen production requires high electric power, and frequent outages interrupt production. The situation has improved immensely now, and outages are addressed instantly, he told Fortune.
"Once the pandemic is over, hospitals will be in better shape to supply oxygen," said Habtamu.
When exactly that will be, however, remains a mystery. More than 60 people have lost their lives to COVID-19 in the past week alone, and 2,258 new cases were recorded. There were 620 people under severe conditions in need of constant oxygen supply for an average of 10 days Frie`s mother had to go through before a recovery.
PUBLISHED ON
May 15,2021 [ VOL
22 , NO
1098]

Radar | Oct 24,2020

Radar | Aug 11,2024

Featured | Sep 23,2023

Commentaries | Jun 15,2019

Life Matters | Jul 17,2022

Radar | Jun 27,2020

Fortune News | Dec 09,2023

Radar | Sep 14,2025

Fortune News | Mar 27,2021

Commentaries | Jan 05,2019

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Nov 1 , 2025
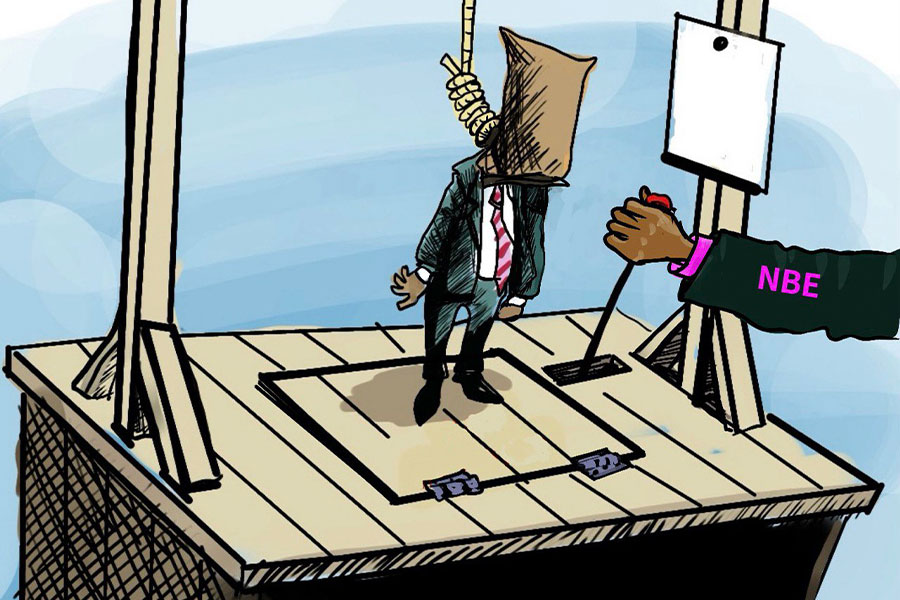
The National Bank of Ethiopia (NBE) issued a statement two weeks ago that appeared to...
Oct 25 , 2025
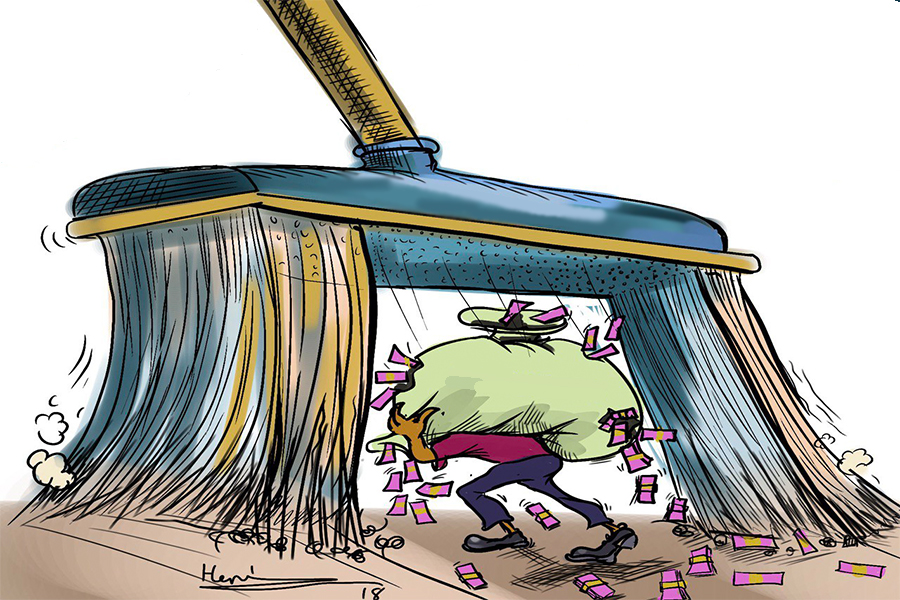
The regulatory machinery is on overdrive. In only two years, no fewer than 35 new pro...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...