
Fortune News | Oct 28,2023
Jun 22 , 2024
By Titir Bhattacharya , Tanika Chakraborty
In recent years, governments in low- and middle-income countries have been experimenting with ways to alleviate the financial burden of high out-of-pocket healthcare costs, accounting for 40pc of household's catastrophic health spending. To ensure universal access, they are gradually shifting away from public provision of health care to publicly funded insurance that covers treatment at private facilities.
India is a prime example. Since the mid-2000s, the central government and various states have introduced such insurance programs to expand healthcare access in low-income communities.
These kinds of public-private partnerships (PPPs) have long been integral to health-policy discussions in developing countries. Since building physical infrastructure is often costly and plagued by bureaucratic delays, political favouritism, and budgetary constraints, national and subnational governments across Asia, Africa, and South America have implemented health insurance schemes enabling low-income families to receive private care at substantially or fully subsidised prices.
The success of these programs varies by country and depends on their design and local context. For example, China and Vietnam are often cited as success stories, with nearly 100pc and 80pcof their populations, respectively, covered by some health insurance schemes as of 2016. But, while out-of-pocket expenses for tertiary care in China have increased, they have decreased following the private-public partnership program's expansion in Vietnam.
India's approach is similar to Vietnam's, focusing on providing the poorest communities with free access to government-funded insurance.
Fully subsidised insurance can improve health outcomes by providing access to private facilities and freeing up space in public hospitals. Yet, despite numerous free insurance programs and high out-of-pocket expenditures, adoption rates in India remain low. Based on data from India's National Family Health Survey, estimates show that just 41pc of Indian households have some form of health insurance. And even those covered seem to have little understanding of how these programs work.
This underscores the importance of the unique context of developing countries, where informal risk-sharing networks traditionally help mitigate the impact of health shocks. In rural areas, households often rely on their local communities and even join groups whose members pool money for health emergencies. Some studies show that the presence of these informal groups can reduce the willingness to pay for formal insurance. While this suggests that informal insurance crowds out formal schemes, our research shows that informal networks might facilitate the widespread adoption of government-provided plans.
For example, the support of such networks can make it easier for people to travel to remote hospitals.
Governments must assess whether the PPP model is the best way to deliver healthcare services. The COVID-19 pandemic has shown that health is a public good with many positive externalities and that direct public provision might be the only feasible option in some cases. Even in less extreme circumstances, it is crucial to understand whether the money spent on one type of program could have been used more effectively elsewhere.
In an ongoing study, we examine the complex implications of the PPP model for healthcare access. In theory, health outcomes might improve if the private system is better than or as good as the public one. But, if the public system is better than its private counterpart, overall health outcomes might be adversely affected. For example, one area where India consistently lags behind its peers is maternal and child health, partly owing to the low rate of hospital deliveries, which in turn can be attributed to the high cost of private services and long wait times in overcrowded government facilities.
If private care were subsidised, more women might choose to deliver their babies in private hospitals instead of non-institutional settings like their homes.
Women often switch from public to private facilities for childbirth following the introduction of a formal health insurance program. Such programs also decrease out-of-pocket expenses, suggesting that individuals who previously paid for private care can now access it at a subsidised rate. Households located far from hospitals, however, remain unaffected by such programs.
Recent estimates from India's National Health Accounts reveal two significant trends: a massive decline in government spending on tertiary health care and a sharp increase in the government's social security expenses, including social health insurance. This reflects the country's shift from direct public provision to the PPP model for tertiary healthcare.
But, if there are too few private facilities, reduced government spending could force people to travel longer distances to access healthcare. Our findings suggest that in Andhra Pradesh, where hospital density is among the highest in India, the difficulty of getting to a hospital – whether monetary or otherwise – affects insurance adoption rates, even when insurance is fully subsidised.
By contrast, Vietnam's success in achieving universal coverage can be partly attributed to substantial public investment in hospitals and health centres.
If India's new social insurance policy leads to the establishment of private hospitals, it could expand access to tertiary healthcare and offset reduced government spending. However, if the growth of these facilities is concentrated in urban areas, far fewer people will benefit. Cultivating PPPs is not enough to make essential healthcare services accessible to all. It is also crucial to ensure that private hospitals are accessible nationwide.
PUBLISHED ON
Jun 22,2024 [ VOL
25 , NO
1260]

Fortune News | Oct 28,2023

Radar | Jan 07,2023

Fortune News | Sep 10,2022

Viewpoints | Mar 09,2024

Radar | Sep 11,2020

Editorial | Aug 30,2025

Commentaries | Sep 08,2024

Fortune News | Jun 01,2019

View From Arada | Aug 27,2022

Fortune News | Dec 29,2018

Photo Gallery | 178426 Views | May 06,2019

Photo Gallery | 168626 Views | Apr 26,2019

Photo Gallery | 159428 Views | Oct 06,2021

My Opinion | 137072 Views | Aug 14,2021
Commentaries | Oct 25,2025

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Oct 25 , 2025
The regulatory machinery is on overdrive. In only two years, no fewer than 35 new pro...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
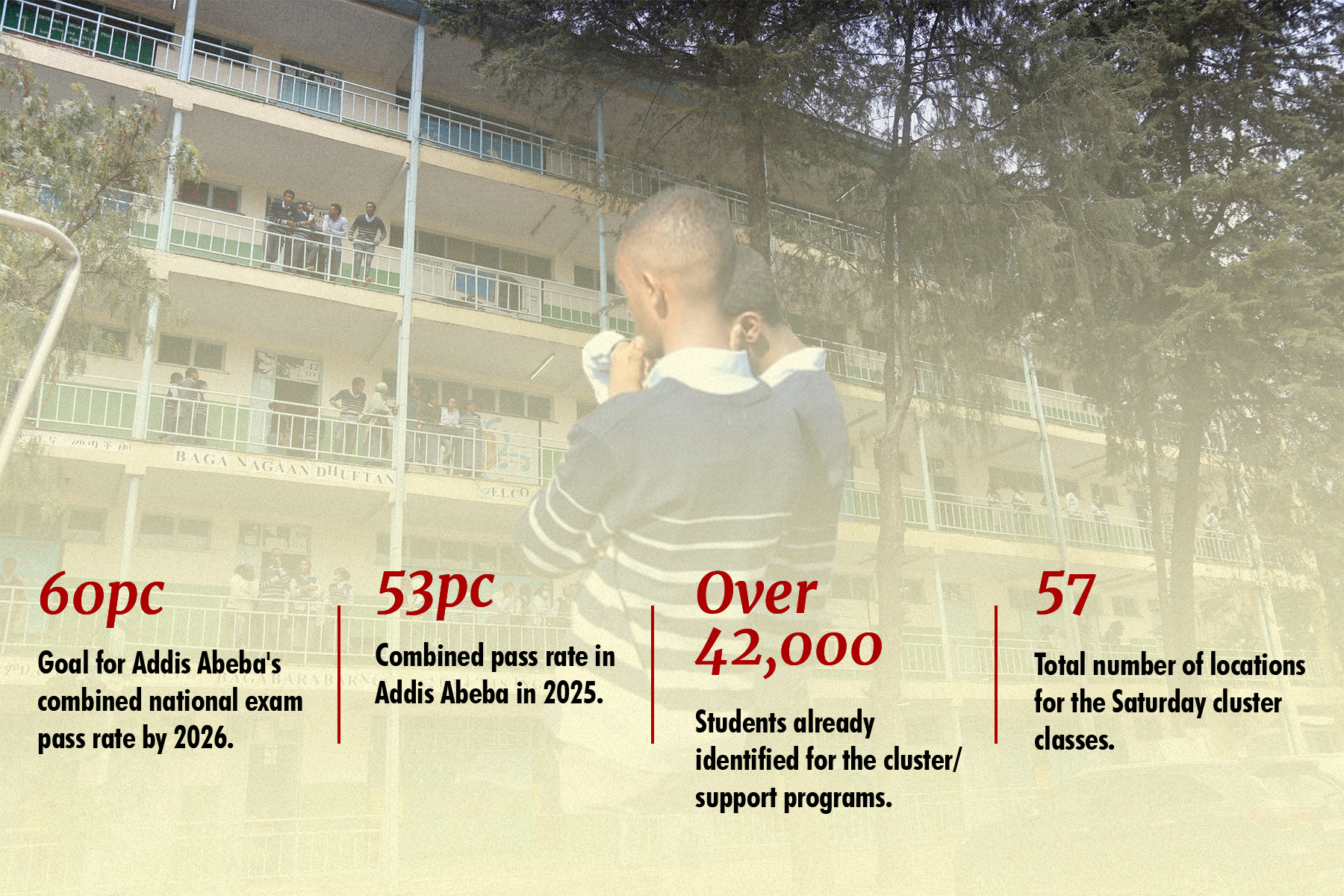
Oct 25 , 2025 . By YITBAREK GETACHEW
Officials of the Addis Abeba's Education Bureau have embarked on an ambitious experim...

Oct 26 , 2025 . By YITBAREK GETACHEW
The federal government is making a landmark shift in its investment incentive regime...

Oct 29 , 2025 . By NAHOM AYELE
The National Bank of Ethiopia (NBE) is preparing to issue a directive that will funda...

Oct 26 , 2025 . By SURAFEL MULUGETA
A community of booksellers shadowing the Ethiopian National Theatre has been jolted b...