
Editorial | May 06,2023
May 11 , 2024
By Nejmudin K. Bilal (MD).
A growing threat could reverse decades of medical advances in Antimicrobial Resistance (AMR). Despite increasing access to essential medicines, it emerges as a silent crisis, with health authorities slow to respond. The World Health Organization (WHO) predicts that if unchecked, AMR could claim 10 million lives annually by 2050. Ethiopia’s battle against this threat is impeded by insufficient implementation of Antimicrobial Stewardship Programs and widespread antibiotic misuse, argues Nejmudin K. Bilal (MD).
Antimicrobial Resistance (AMR) is emerging as a silent crisis in Ethiopia. While striving to improve access to essential medicines, the country has inadvertently neglected a growing threat that could undermine decades of medical gains. Despite the significance of AMR as a global health crisis, health authorities' response has been tepid, risking severe future repercussions for the healthcare system and economy.
Predictions from various studies suggest that, if unchecked, the AMR crisis could claim 10 million lives annually by 2050 and impose a global economic burden of about 100 trillion dollars. The impact of AMR extends beyond health, affecting socio-economic development across the continent, a risk acknowledged by the African Union (AU) in its endorsement of the African Common Position on Controlling Antimicrobial Resistance.
The stakes are particularly high in Ethiopia, a country with a population of over 100 million and a heavy burden of infectious diseases. However, several factors have constrained its leaders' efforts to combat AMR.
The Ministry of Health (MoH) introduced a guideline in 2018 to establish an Antimicrobial Stewardship Program in hospitals, yet this program has not been widely implemented. Poor infection prevention practices among healthcare workers and the unregulated over-the-counter prescription of antibiotics continue to aggravate the situation. A considerable proportion of antibiotic prescriptions — up to half, according to some estimates — are unnecessary, uncovering the rampant misuse of these critical drugs.
The economic implications of AMR are also substantial. A study focusing on treating pneumococcal disease in children estimated the annual costs associated with AMR at around 15.8 million dollars. This includes 3.3 million dollars spent on ineffective first-line treatments, an additional 400,000 dollars on second-line treatments, and another 8.9 million dollars lost due to long-term productivity declines.
The national strategy for AMR is underdeveloped, and there is a notable lack of comprehensive data to understand the problem's magnitude or monitor trends effectively. This data deficiency inhibits making informed decisions and implementing effective interventions.
The federal government has made strides in encouraging the domestic and overseas manufacture of pharmaceuticals, leading to a burgeoning market worth between 400 million dollars and half a billion dollars a year by 2016, growing by a quarter annually. Approximately 12 pharmaceutical companies and about 200 importers of pharmaceutical products and medical consumables were operational. While these efforts have been directed towards improving access to medicines, they inadvertently overlook the critical issue of AMR due to the excessive and inappropriate use of antimicrobials.
Addressing AMR requires various approaches. Gathering and analysing data to grasp the full extent of AMR and track emerging trends is essential. Such data is crucial for tailoring interventions and assessing their effectiveness. Substantial investments are needed to implement antimicrobial stewardship programs effectively. These programs should focus on improving infection prevention practices, updating therapeutic guidelines, enhancing the skills of health professionals, and educating the public about rational drug use.
Regulatory oversight is another critical component. Effective regulation can ensure that policies, strategies, and guidelines are well-crafted and faithfully executed. This includes tightening controls over the prescription of antibiotics in both public and private healthcare settings. The issue of AMR also demands a coordinated response across various sectors, not just the health sector. Federal health officials could prioritise advocacy and engage with other sectors directly impacted to address the AMR crisis comprehensively.
While some may argue that focusing on AMR might divert resources from efforts to achieve universal health coverage, it is essential to recognise that these objectives are not mutually exclusive. Implementing programs to counter AMR can go along with expanding access to healthcare. Indeed, the benefits of antimicrobial stewardship programs, which include preserving the effectiveness of existing drugs and reducing healthcare costs, far outweigh the initial resource allocation required to establish and maintain them.
It should be urgently recognised that Ethiopia faces daunting problems in addressing antimicrobial resistance. This challenge cannot be ignored. Without a meaningful effort to understand and combat AMR, its population risks a consequential setback to its health and economic progress. The time to act is now, with a clear focus on data collection, regulatory enforcement, and multisectoral cooperation to forge a sustainable response to a convoluted global health threat.
PUBLISHED ON
May 11,2024 [ VOL
25 , NO
1254]


Editorial | Dec 30,2023

Editorial | Feb 18,2023

Commentaries | Jan 03,2021

Featured | Aug 22,2020

Radar | Jul 13,2019

Photo Gallery | 175385 Views | May 06,2019

Photo Gallery | 165605 Views | Apr 26,2019

Photo Gallery | 155938 Views | Oct 06,2021

My Opinion | 136814 Views | Aug 14,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
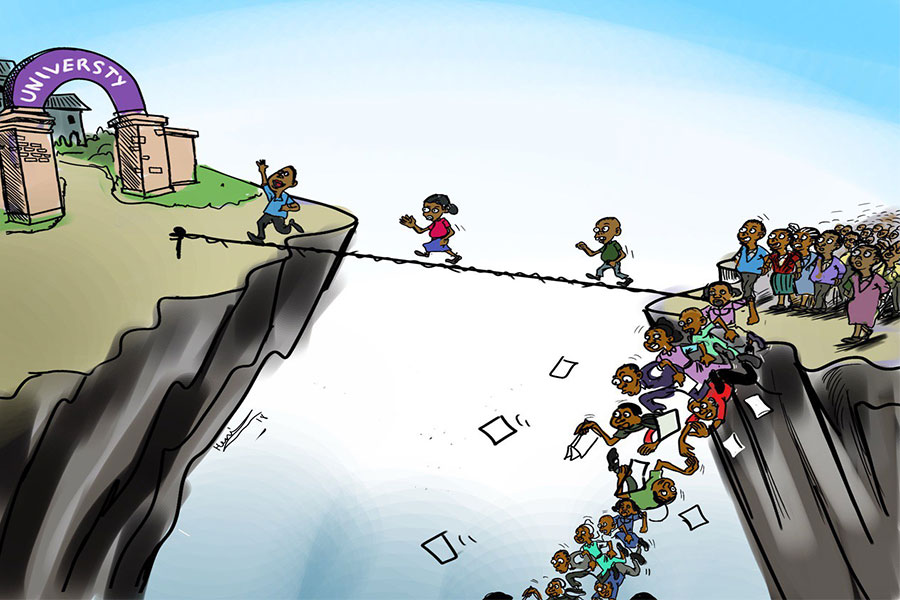
Four years into an experiment with “shock therapy” in education, the national moo...
Oct 18 , 2025 . By NAHOM AYELE
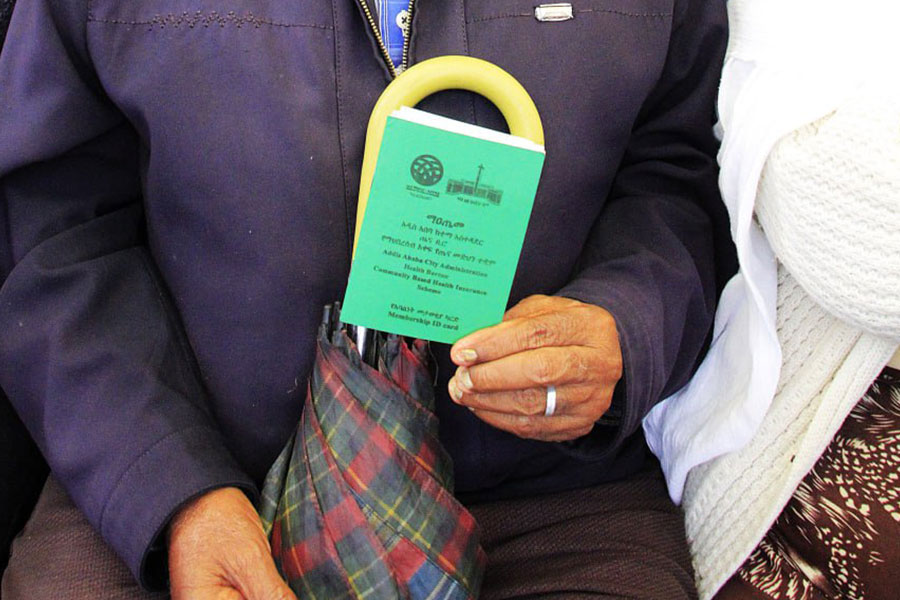
In a sweeping reform that upends nearly a decade of uniform health insurance contribu...

Oct 18 , 2025 . By BEZAWIT HULUAGER
A bill that could transform the nutritional state sits in a limbo, even as the countr...

Oct 18 , 2025 . By SURAFEL MULUGETA
A long-planned directive to curb carbon emissions from fossil-fuel-powered vehicles h...

Oct 18 , 2025 . By BEZAWIT HULUAGER
Transaction advisors working with companies that hold over a quarter of a billion Bir...