
Commentaries | Jan 23,2021
May 18 , 2019
By Dawit Wondimagegn
Over the past decade, Ethiopia’s health system has deteriorated, neither meeting social expectations of the public nor the professional requirements of its practitioners, writes Dawit Wondimagegn (MD) (dawitwondimagegn@gmail.com), associate professor of psychiatry at Addis Abeba University’s School of Medicine and chief executive director of Tikur Anbessa Hospital. His views are personal and do not represent the opinion of any institution.
It is not uncommon for Ethiopia’s health system to be described as neither meeting social expectations of the public nor the professional requirements of its practitioners. Having been engaged in the sector for almost a quarter of a century, including seven and a half years in medical school, I have had the opportunity to observe how a poor but well organized and functional health system slowly spiraled into crisis.
Society’s priorities have been shifting over the last three decades. Primarily, the ideals of interdependence and community have gradually changed toward the ideals of autonomy and independence. This would not have been an issue had the promises of globalization, the creation of a just and equitable world where we all live together, proved true.
Instead, the creation of a “pseudo autonomous and independent self” meant professionals are no longer governed by the rules, norms and customs of the very society that created them, effectively annihilating individuals from the fabric of society. The very people society expects to solve its problems have become the problem.
What does this mean for health care?
In the past, the foundational priority of health care used to be “serving society.” This priority has shifted to the imperative that health care is an economic opportunity.
The strong influences of the market gradually eroded the age-old purpose of medicine - the good of the patient.
Health care as an economic opportunity may or may not be viable. Reality prevails and context matters. It is in the above background that we need to see our health system. Any health system needs to fulfill four aims to survive the new age.
Primarily, it needs to make the experience of health care positive. This means it has to satisfy its consumers - patients. Irrespective of reasons, our record has been dismal with regard to patient satisfaction.
The crisis of trust in the health system is at its peak. Public trust in the health system has been fading away. The health policy framework, health professionals, the media and the public at large have played and still play significant roles in diminishing the already dwindling trust the public has in the health system in general and health professionals in particular. Health professionals, in most circumstances, are the scapegoats for systemic failures.
A health system should also aim to improve the health of a population. This needs a strong technocracy that continually identifies population-level health issues and puts the necessary strategies in place to address them. Our health system, which is “a technocracy without technocrats” has been and still is ill-equipped to come up with strategies that address population needs.
We have been trying to find a population with a need that fits our policy and strategy instead of forming policies and strategies that fit the population's needs. A glaring example is excessive, albeit appropriate, focus on preventive strategies. This is despite strange and utter neglect and absence of policies on improving curative services, resulting in tertiary care that struggles to exist with its own devices and paradoxically refuses to die despite systemic attempts to do so.
Just as importantly, a health system should aim to deliver care at a low cost. Health care is expensive. Providing just the basic necessities requires a fortune and wise investment. As a developing nation, although we live on meagre resources, our spending in the health system has been far from wise. We probably have one of the most expensive health systems relative to its outcomes.
The amount of redundancies and fragmentation in investment and human capital bleeds the hearts and souls of many well-meaning citizens. The organization of health services is too disorganized.
The misguided focus on meeting irrelevant standards meant so much money and time is invested in creating an unnecessary and excessive regulatory mechanism where regulation became the mainstream activity instead of health services. Most health institutions focus on meeting regulatory expectations rather than meeting the health outcomes of patients.
It is commonplace to see patients lying on the floors of one hospital, while another hospital prides itself by claiming it has 20pc of its beds free just to meet an 80pc bed-occupancy ratio according to the “standard”. We have a good example of a system that meets "reporting" criteria rather than real criteria! Instead of aiming for low-cost care, we managed to create a costly one, paying with human life.
Lastly, a health system should aim to protect the health of its health professionals. Every system is as good as it is. What it is is people. Individuals make systems. This makes the presence of a healthy workforce not only necessary but pivotal for ensuring success in all other aims that the health system aspires to fulfill.
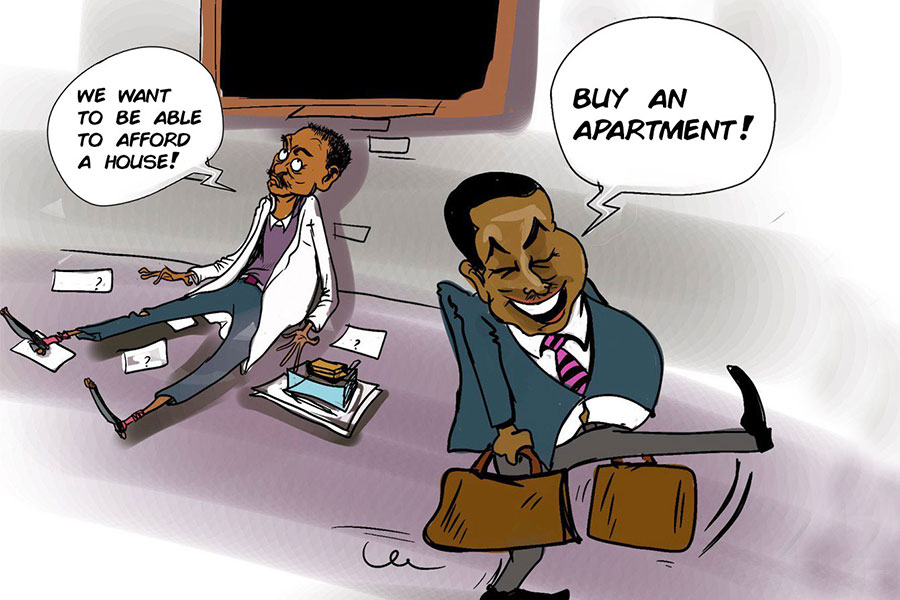
Unwise, emotional, irresponsible and short-sighted decisions in human resource development over the last 15 years has created under-trained, overworked, underpaid, overwhelmed and frustrated health workers to such an extent that now the entire health system is under enormous stress. The famous policy of “flooding” the country with unemployed doctors may have fulfilled its purpose. Indeed, we are now a nation that affords not to employ its doctors, not because there are enough of them, but because it cannot afford them!
Many regrettable decisions had been made in the name of improving the health and life of our people. It is true that many lives have improved. Many of these decisions were also made to deal with some crisis like human resources, capital and supplies. Undoubtedly, there have been perceptible differences made. But these successes are too far apart, and the health of our people has been led into a spiral of crisis.
That is the tale of our health system. It is not easy to meet the four aims mentioned above, but it is not difficult. This does not call for reinventing the wheel. We need to look inwards and explore where improvements can be initiated.
What do our patients need when they come for care? What are the health needs of the population and what policy and strategy will best fit that need than the other way around? What is the cheapest way to deliver care? How about the health of health professionals?
We know the answer. We have data. We live with people. All that is required of us is to come out of the illusion that we are creating society. Society is there to be served. Society has invested in us to come up with solutions, not to reformulate society as the problem.
We also need to avoid redundancies to deliver cheaper care. We need to move from reporting to delivering and organise a fragmented health system through meaningful integration.
As for the health of health professionals, a mechanism to prevent, identify and act on issues that are close to the hearts and minds of professionals should be created. Health professionals, by large, are reasonable people but people nonetheless. They have needs and wants. As long as these are being taken care of in a systemic fashion, they will only follow what their good hearts tell them. At the bottom of their heart, there is only care. Where ever humanity is loved, health professionals are there, albeit as mere humans.
In nations like ours, a crisis is more of a norm than an exception. The fact that we are in a spiral of crisis is not a problem in and of itself, but it becomes a problem in a world with constantly shifting ideals toward independence and autonomy. This is because interdependence has always been the thread that held, and is still holding, society at times of crisis. With the loosening of interdependence, it is only natural for people to look out only for oneself and at oneself.
The crucial step for our health system to come out of this spiral is through a concerted acknowledgement of the interdependence of society.
PUBLISHED ON
May 18,2019 [ VOL
20 , NO
994]


Commentaries | Jan 23,2021

Viewpoints | Aug 10,2024

Fortune News | Jul 08,2023

Radar | Oct 31,2022

Radar | May 04,2024

Fortune News | Aug 05,2023

Commentaries | Jul 10,2021

Fortune News | Jul 17,2022

Radar | Feb 06,2021

Viewpoints | Apr 19,2025

My Opinion | 131499 Views | Aug 14,2021

My Opinion | 127855 Views | Aug 21,2021

My Opinion | 125833 Views | Sep 10,2021

My Opinion | 123463 Views | Aug 07,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Jun 28 , 2025
Meseret Damtie, the assertive auditor general, has never been shy about naming names...

Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...

Jun 14 , 2025
Yet again, the Horn of Africa is bracing for trouble. A region already frayed by wars...
Jun 7 , 2025
Few promises shine brighter in Addis Abeba than the pledge of a roof for every family...

Jun 29 , 2025
Addis Abeba's first rains have coincided with a sweeping rise in private school tuition, prompting the city's education...

Jun 29 , 2025 . By BEZAWIT HULUAGER
Central Bank Governor Mamo Mihretu claimed a bold reconfiguration of monetary policy...

Jun 29 , 2025 . By BEZAWIT HULUAGER
The federal government is betting on a sweeping overhaul of the driver licensing regi...

Jun 29 , 2025 . By NAHOM AYELE
Gadaa Bank has listed 1.2 million shares on the Ethiopian Securities Exchange (ESX),...