Editorial | Jun 29,2024
Jan 27 , 2024
By Benjamin Schreiber , Richard Mihigo and Ann Lindstrand
There was a global sigh of relief when the World Health Organization (WHO) declared in May last year that COVID-19 was no longer a public health emergency of international concern. But there is no room for complacency. The pandemic has represented an urgent warning about weak health systems and has served as an impetus to strengthen them ahead of a possible new variant or the emergence of a new pathogen.
The challenges of vaccine delivery, in particular, offered insights into what makes a successful health campaign. Specifically, lower-income countries demonstrated how to reach people where they are by using innovative and tailored approaches that often required collaboration among national governments, local organisations, and vulnerable communities. Their experience provides crucial lessons as the world prepares for the next pandemic.
Like their wealthier counterparts, lower-income countries had to vaccinate their adult populations against COVID-19 as quickly as possible. That meant reaching broader population groups than their existing childhood vaccination programs could serve while also targeting those in the greatest need: healthcare workers, immunocompromised people, and the elderly.
But lower-income countries faced unique challenges.
Owing to vaccine nationalism and other obstacles, many of them only accessed consequential amounts of doses much later than high-income countries, delaying their immunisation campaigns. A dearth of financial resources, together with the weaknesses of national health systems, also hindered vaccine uptake. For example, countries with limited cold-chain capacity often lacked the ultra-cold storage facilities required for certain COVID-19 vaccines. Many countries' reporting systems could not provide decision-makers with up-to-date, in-depth data to adjust rollout strategies based on what was working and what was not.
Despite these challenges, lower-income countries found ways to meet the needs of their communities. These initiatives included door-to-door outreach to vaccinate older people at home; female vaccination teams to encourage uptake by women; coordination between professional organisations and the private sector to reach people at the highest risk of getting very sick from COVID-19; mobile vaccination teams – on buses, motorbikes, camels, donkeys, and boats – to access remote or underserved areas; and vaccination sites in markets, along nomadic routes, and at major transit points, including bus stations.
Somalia is a good example of how to reach people where they are.
The vaccine rollout occurred in the context of multiple overlapping challenges of years-long political instability and conflict; severe hunger caused by the worst drought in decades; and the displacement of several hundred thousand people by historic floods. But, the country's polio vaccination program had pioneered the use of locally informed "micro-planning" to find unvaccinated people, and these tailored strategies ensured that Somalia's nine mass COVID-19 vaccination campaigns reached underserved populations, such as women and nomadic communities.
In September-October 2022, for example, a phased campaign led by the Somali government reached 3.2 million people, achieving a 37pc primary series vaccination rate. Equally important was Somalia's investment in cold-chain infrastructure and vaccine-delivery logistics, made possible with financial support from partner organisations.
The Solomon Islands, the South Pacific's third-largest archipelago, also struggled to vaccinate people living in remote areas, given that most of the country's resources are concentrated on Guadalcanal, the largest island. Government health workers responded by creating pop-up and informal clinics on outer islands, making it easier for isolated communities to receive the COVID-19 vaccine and additional health services.
In Sierra Leone, a country covered by grassland, savannah, and dense forest, many villages can be reached only by bike or on foot – a journey made even harder during the rainy season. However, the country's health workforce, together with community mobilisers, conducted mobile vaccination clinics in rural villages. To address fears about the vaccine, local leaders took the jab and then promoted their vaccinated status within the community, creating a snowball effect.
In Mali, access to information similarly posed a major challenge, as many people were not aware of the availability or effectiveness of the COVID-19 vaccine. To engage communities and raise awareness, trucks carrying entertainers and influencers alongside vaccinators travelled through busy markets to answer questions and encourage passers-by to get the shot; loud music and dancing created a buoyant atmosphere. Over 12 days, the caravan reached more than 21,000 people and vaccinated more than 3,000 men, women, and adolescents.
These innovative strategies can serve as models for the global community. But they also highlight the importance of developing tailored immunisation programs, which in turn require trust, clear communication, equitable access to vaccines, data-driven decision-making, and collaboration among governments, health organisations, grassroots groups, and volunteers.
In the wake of the COVID-19 pandemic, we know that miraculous vaccines can be developed quickly and delivered to hard-to-reach communities. The key is to focus on meeting people where they are.
PUBLISHED ON
Jan 27,2024 [ VOL
24 , NO
1239]
Editorial | Jun 29,2024

Commentaries | Sep 23,2023
Radar | May 23,2020
Editorial | Oct 15,2022

Radar | Nov 20,2023

Covid-19 | Jan 23,2021

Viewpoints | Mar 05,2022

Viewpoints | Jul 30,2022

Viewpoints | Nov 29,2020

Radar | Apr 17,2021

My Opinion | 131499 Views | Aug 14,2021

My Opinion | 127855 Views | Aug 21,2021

My Opinion | 125833 Views | Sep 10,2021

My Opinion | 123463 Views | Aug 07,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Jun 28 , 2025
Meseret Damtie, the assertive auditor general, has never been shy about naming names...
Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...

Jun 14 , 2025
Yet again, the Horn of Africa is bracing for trouble. A region already frayed by wars...
Jun 7 , 2025
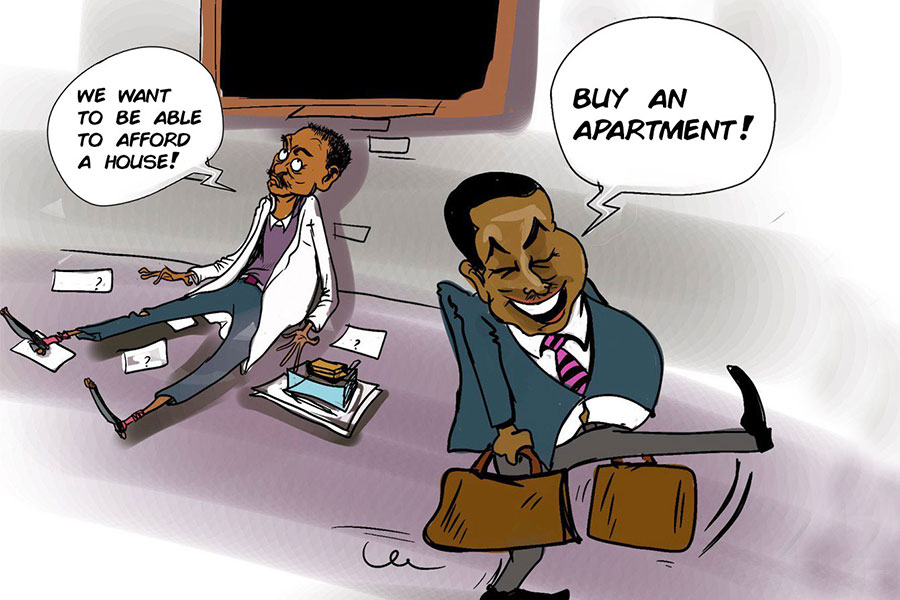
Few promises shine brighter in Addis Abeba than the pledge of a roof for every family...

Jun 29 , 2025
Addis Abeba's first rains have coincided with a sweeping rise in private school tuition, prompting the city's education...

Jun 29 , 2025 . By BEZAWIT HULUAGER
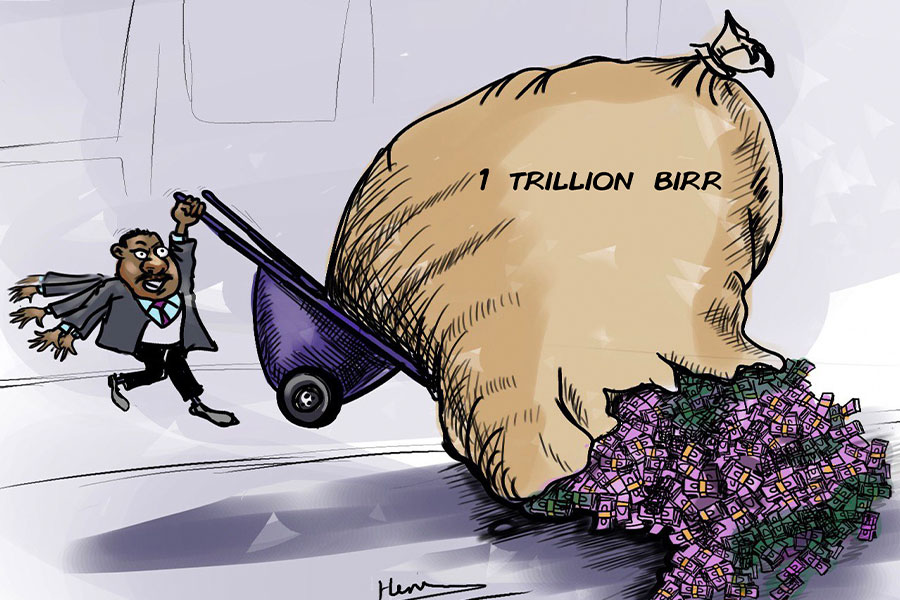
Central Bank Governor Mamo Mihretu claimed a bold reconfiguration of monetary policy...

Jun 29 , 2025 . By BEZAWIT HULUAGER
The federal government is betting on a sweeping overhaul of the driver licensing regi...

Jun 29 , 2025 . By NAHOM AYELE
Gadaa Bank has listed 1.2 million shares on the Ethiopian Securities Exchange (ESX),...