
Apr 19 , 2025. By Ifeanyi M. Nsofor ( Ifeanyi M. Nsofor, a senior new voices fellow at the Aspen Institute, i )
African countries face urgent health problems, from rising noncommunicable diseases (NCDs) to the persistent threat of malnutrition. As foreign aid contracts, leaders should move towards healthy policies that boost domestic revenue, like taxing sugary drinks to curb obesity and diabetes. Finding fiscal solutions like these, paired with the strategic use of diaspora remittances, can unlock billions in funding, steering the continent toward a healthier, self-sustained future, argued Ifeanyi M. Nsofor, a public health physician and behavioural science researcher. This commentary is provided by Project Syndicate (PS).
A global storm is gathering, and Africa is directly in its path. Under President Donald Trump, the United States has frozen 40 billion dollars in USAID funding, slashing 83pc of grants. European donor countries are also drastically cutting their foreign-aid commitments, signalling a broader shift in priorities. The devastating effects are already being felt across Africa, particularly in sectors like healthcare, education, and social services, which have long relied on external support.
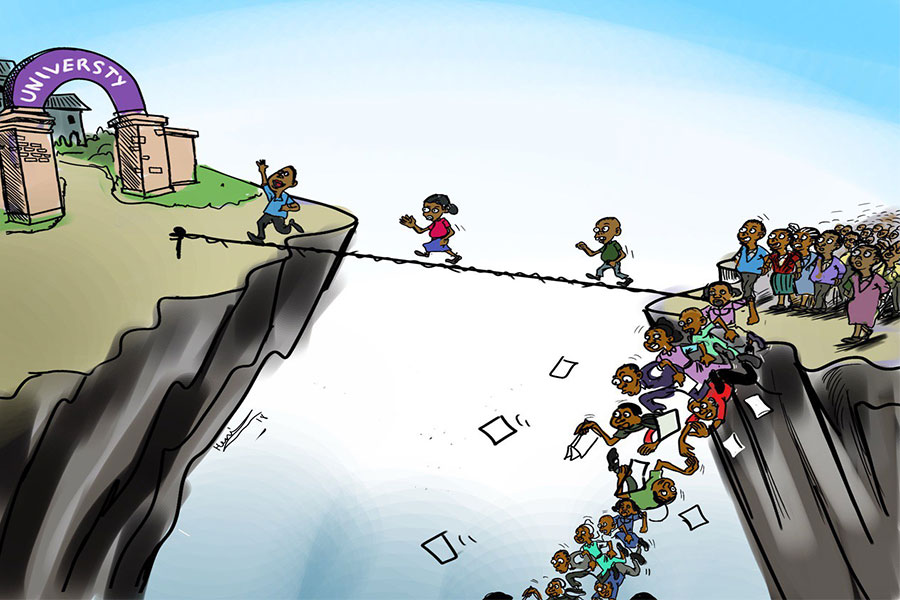
For decades, African governments have depended heavily on foreign aid, often at the expense of building sustainable domestic financing systems. But the current wave of aid cuts proves an uncomfortable truth: foreign aid is inherently unreliable. It can be paused, reduced, or redirected at any time, without warning, and is often subject to political shifts in donor countries.
The current financial crisis, then, should serve as a wake-up call. African countries should reclaim control of their futures by adopting bold, innovative strategies to close funding gaps and build resilient, self-sufficient health systems.
African governments should invest in homegrown financing solutions for essential public services. In the health sector, the main focus should be achieving universal health coverage through a robust, well-funded primary health care (PHC) system. Most donor-funded health initiatives – vaccinations, childcare, nutrition, sanitation, and disease control – fall squarely within the PHC framework. According to the World Health Organisation (WHO), up to 90pc of an individual's healthcare needs can be addressed at the PHC level.
Focusing on prevention and health promotion thus remains the fastest and most cost-effective way to improve health outcomes across Africa. Preventive PHC measures such as childhood vaccinations, hypertension screenings, prenatal care, and nutrition services could significantly reduce mortality rates among mothers and children under five. Malnutrition alone contributes to nearly half of all deaths among children in this age group, underscoring the urgent need for early, community-based care.
Unfortunately, more than four decades after the 1978 Alma-Ata Declaration defined PHC as the foundation of equitable health care, many of its goals remain unfulfilled. Consequently, African governments should develop independent health financing mechanisms to ensure long-term accessibility and accountability.
Health insurance represents an opportunity for African countries to draw on their cultural traditions of collective responsibility and community-based support. South Africa's Zulu people live by the principle of Ubuntu – "I am because you are" – while the Igbo people of Nigeria uphold Ìgwèbíké ("strength in unity"). These deeply rooted values mirror the essence of health insurance. Protect individuals by pooling resources.
Rwanda and Morocco offer compelling models for strengthening PHC systems and expanding access. Rwanda's community-based health insurance, rolled out nationwide in 2004, now covers more than 90pc of the population, making it one of Africa's most effective health financing models. The scheme is funded through a combination of member premiums, government contributions, international donors, and other mechanisms. It is also supported by roughly 59,000 community health workers, who serve as vital links between households and formal services.
Over the past two decades, the program has reduced financial barriers and decentralised service delivery, bringing health care to the communities that need it most.
In Morocco, the government introduced a dual national health insurance system in 2005: Assurance Maladie Obligatoire (AMO) for workers in the formal sector and Régime d'Assistance Médicale) for informal workers. In 2022, these programs were consolidated into the AMO-Tadamon program, enabling beneficiaries to access public and private facilities. This reform not only eased pressure on public health facilities but also promoted equitable access through strategic financing, with insurance coverage surging from just 15pc in 2005 to nearly 80pc today. In 2023, the World Bank approved a 450-million-dollar program-for-results loan to advance universal health coverage in Morocco and increase access to quality care.
The need for universal coverage in Africa is particularly urgent as the continent faces a surge in noncommunicable diseases (NCDs), including hypertension, heart disease, diabetes, and cancer. Collectively, these disease types – driven by unhealthy diets, sedentary lifestyles, and excessive alcohol and sugar consumption – claim 41 million lives annually, with 32 million deaths occurring in low- and middle-income countries.
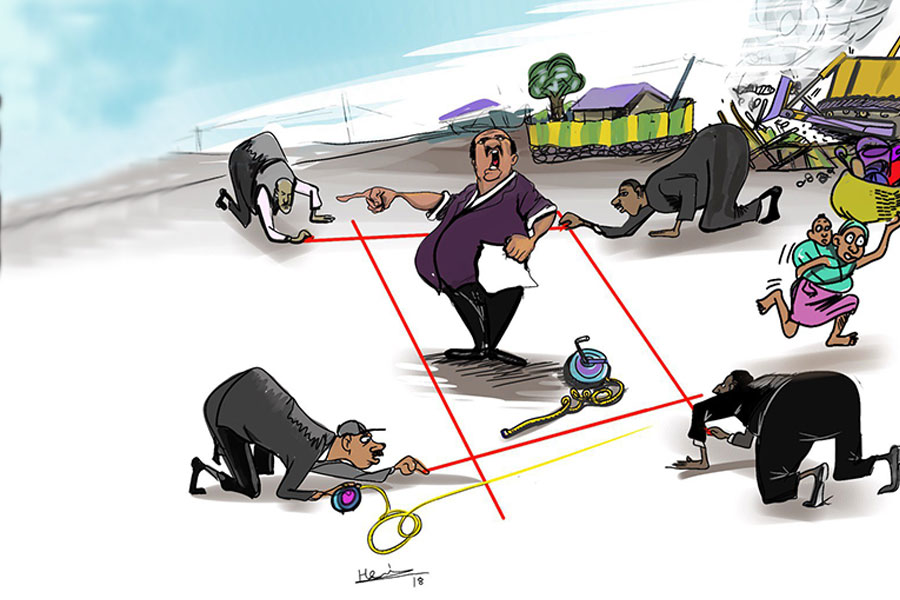
As foreign aid shrinks, African leaders should adopt bold policies that encourage healthier lifestyles and boost domestic revenue. One such solution is taxation. As the WHO's Sugar Tax Report shows, taxing sugary beverages reduces consumption and lowers the risk of obesity and diabetes. Experts at the recent Global NCD Alliance Forum underscored the need for stronger excise taxes across Africa to curb the growing NCD epidemic and generate sustainable revenue streams for public health investments.
South Africa and Mexico demonstrate the promise of such measures. Mexico implemented a one-peso-per-liter excise tax on sugar-sweetened beverages on January 1, 2014, and consumption of sugary drinks fell by 7.6pc over the two-year period between 2014 and 2015. In South Africa, a 2018 sugar tax led to a 51pc reduction in purchases of sugary drinks, 52pc reduction in calories, and 29pc reduction in the volume of beverages purchased per person a day.
Diaspora remittances represent a promising and sustainable source of funding. While talent continues to leave Africa, remittances also create a powerful "brain gain," delivering a stable flow of funds to the continent. In 2024, remittances to Africa exceeded 100 billion dollars, outpacing foreign aid. Diaspora Nigerians alone accounted for 20pc of this figure. Globally, remittances reached 590 billion dollars in 2020, far surpassing official development assistance, which stood at 180 billion dollars, and philanthropic outflows, which totalled 70 billion. dollars.
If African countries had allocated one percent of every remittance dollar to health insurance – as I proposed in 2019 – the 100 billion dollars in remittances sent by the African diaspora in 2024 could have generated one billion dollars for health care, bringing the continent closer to achieving universal health coverage. But to unlock the remittances' full potential, African governments should improve governance, strengthen accountability, and promote trust with diaspora communities.
Of course, Africa is not a monolith. Solutions should be tailored to each country's unique context, complementing broader efforts to boost domestic resource mobilisation. What is clear, however, is that lasting independence depends on financial self-reliance. For African countries to control their financial futures, they should ensure that they can fund essential services like healthcare without relying on external support.
PUBLISHED ON
Apr 19,2025 [ VOL
26 , NO
1303]

Photo Gallery | 173747 Views | May 06,2019

Photo Gallery | 163973 Views | Apr 26,2019

Photo Gallery | 154017 Views | Oct 06,2021

My Opinion | 136569 Views | Aug 14,2021

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
Four years into an experiment with “shock therapy” in education, the national moo...
Sep 20 , 2025
Getachew Reda's return to the national stage was always going to stir attention. Once...