
Photo Gallery | 174811 Views | May 06,2019
Jan 1 , 1970
By Halima Abate (MD)
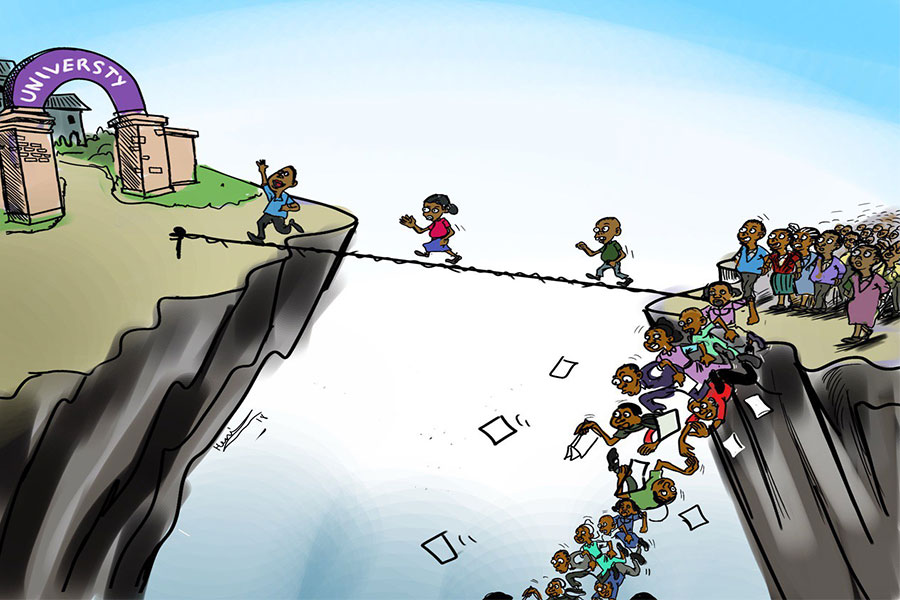
Ethiopia's efforts to build a robust and accessible healthcare system face a severe roadblock, primarily driven by disabling shortages and management issues within its human resources sector. As the country works toward achieving Universal Health Coverage (UHC), persistent brain drain and recent cuts to crucial foreign aid threaten to reverse the hard-earned progress.
Doctors, nurses, and healthcare specialists increasingly seek opportunities abroad, drawn by higher wages, improved working conditions, and better professional growth. Domestically, they face poor pay, heavy workloads, inadequate resources, and limited career advancement opportunities. Political and economic instability adds another layer of uncertainty, further motivating health workers to pursue careers elsewhere.
Recent cuts in USAID funding have intensified these problems. Reduced foreign aid directly affects salaries, training programs, and vital infrastructure projects. The reduction has resulted in job losses across the health sector, deepening the understaffing crisis. Fewer training programs and limited medical resources also compromise patient care, burdening already overstretched facilities.
Recognising this, the federal government introduced a strategic plan for the national human resource for health (HRH), whose shelf life is to end this year. The ambitious program sought to address workforce shortages, geographic distribution disparities, and skill gaps in healthcare personnel. Assessing its successes and shortcomings has become essential as the initiative nears its conclusion.
The plan delivered some encouraging outcomes, including an expansion of the health workforce, targeted recruitment for underserved regions, and initiatives to build healthcare capacity. Task-shifting programs, designed to optimise available staff, also marked a noteworthy step forward. Nevertheless, major constraints remain largely unaddressed. Workforce shortages in rural areas persist, and retaining experienced professionals is problematic.
Quality education and training programs for health professionals require substantial improvement. Graduates often emerge ill-equipped to manage contemporary healthcare demands, creating additional pressure within an already strained system. Urban-rural disparities persist, disproportionately affecting rural regions by workforce shortages and limited healthcare accessibility. Inadequate governance, planning, and resource allocation undermine effective management and coordination of the healthcare workforce.
Despite attempts to address these issues, health authorities' limited financial resources constrain the comprehensive execution of the strategic plan. They need targeted interventions to address the damaging effects of brain drain and declining aid. Foremost among these is boosting domestic healthcare investment. Allocating a larger portion of the federal budget specifically for healthcare, including salaries, training, and infrastructure, is essential to mitigate reliance on external funding.
Improving workforce retention remains a crucial priority. Offering competitive salary packages, enhancing working conditions, and providing clear pathways for career growth would encourage healthcare professionals to stay in Ethiopia. Tailored strategies meeting the unique needs of rural healthcare workers could alleviate workforce imbalances and attract professionals to underserved areas.
Diversifying funding sources is equally critical. Encouraging public-private partnerships, creating innovative financing mechanisms, and raising domestic revenue could lessen the dependence on international assistance. Technological innovation presents additional opportunities. Telemedicine, for instance, offers the potential to bridge gaps in rural healthcare access. Remote monitoring, virtual consultations with specialists, and online training could revolutionise healthcare delivery, especially in isolated areas lacking adequate facilities.
Enhancing policy frameworks and governance practices is another vital step. Strengthening regulatory oversight, improving data collection, and ensuring transparency are necessary to optimise healthcare resource management. Effective governance will facilitate better resource allocation and enhance accountability, thereby improving overall health outcomes.
Educational reforms are no less important to ensure that healthcare graduates are adequately prepared. Curriculum improvements, increased investment in faculty training, and the adoption of innovative teaching methods will help graduates meet the evolving demands of the healthcare sector. The strategic plan may have laid the groundwork for addressing these issues. However, sustaining progress requires ongoing investment, innovative strategies, and robust governance. Without addressing these fundamental issues, Ethiopia's ambitions for universal health coverage may falter.
PUBLISHED ON
30, 2025 [ VOL
25 , NO
1300]


Photo Gallery | 174811 Views | May 06,2019

Photo Gallery | 165032 Views | Apr 26,2019

Photo Gallery | 155285 Views | Oct 06,2021

My Opinion | 136727 Views | Aug 14,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
Four years into an experiment with “shock therapy” in education, the national moo...
Oct 18 , 2025 . By NAHOM AYELE
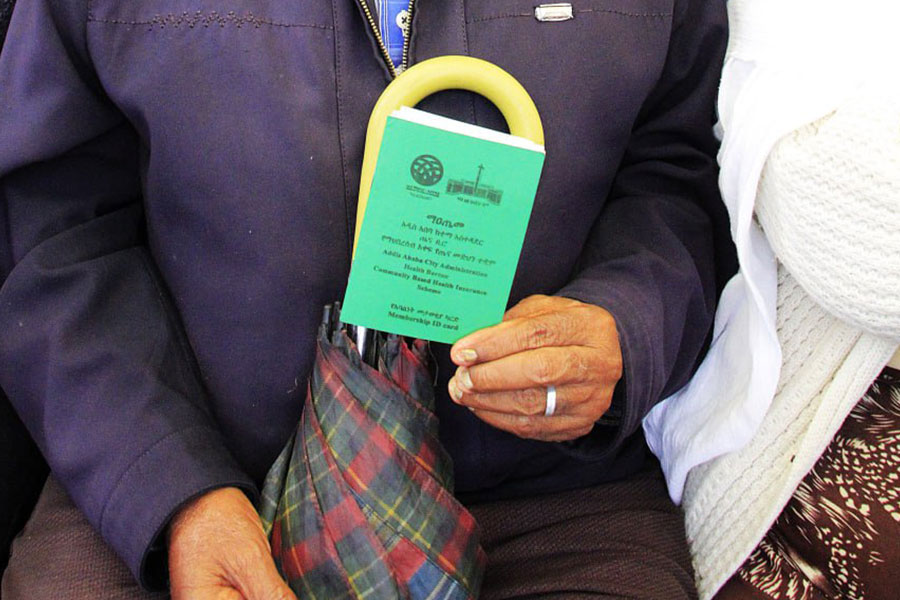
In a sweeping reform that upends nearly a decade of uniform health insurance contribu...

Oct 18 , 2025 . By BEZAWIT HULUAGER
A bill that could transform the nutritional state sits in a limbo, even as the countr...

Oct 18 , 2025 . By SURAFEL MULUGETA
A long-planned directive to curb carbon emissions from fossil-fuel-powered vehicles h...

Oct 18 , 2025 . By BEZAWIT HULUAGER
Transaction advisors working with companies that hold over a quarter of a billion Bir...