
Radar | Jul 24,2021
Dec 26 , 2020
By Bjorn Lomborg
In the next two minutes, one woman will die from complications related to pregnancy and childbirth. She will die from entirely preventable causes during one of the most beautiful moments of human life — giving birth. The good news is that there are some solutions that are inexpensive and effective.
In a world besieged by problems from COVID-19 to climate change, it is hard to pay attention to the many other challenges that still remain. For the vast majority of the world's population, these are simple problems of survival: not dying from tuberculosis, getting enough food, breaking free of poverty and getting an adequate education.
Vying for scarce resources, these problems often lose out, because they do not get enough media attention, famous spokespeople or viral imagery. The harsh truth is we cannot afford to fix all problems.
That is why we have to ask hard questions: how big is the problem, what is the solution — and crucially, how much will it cost compared to its effects?
The tragedy of pregnant women and their children dying has been on the global health community's radar for a long time. Twenty years ago, the UN promised to address the issue. But progress to date has not been enough. Yes, maternal deaths declined about a third from 451,000 per year in 2000 to about 295,000 today, but we had committed to more than a two-thirds reduction by 2015. Since then, we have promised to reduce it even further to around 100,000 deaths by 2030.
But commitment without action does not save pregnant women and their children. It takes financing and simple procedures.
Mothers in the hardest-hit developing countries are still 80 times more likely to die than their rich-country counterparts. And their newborns also die — last year 2.4 million children died in their first 28 days on earth. They die because many women either give birth in their own homes, without access to skilled birth attendants or in facilities with limited basic emergency care. The mothers die from infections that abound with low hygiene and high blood pressure that can lead to seizures. Severe bleeding that can happen after childbirth kills 46,000 mothers every year.
Clearly, something needs to be done. Development professionals have put forward many proposals on how to address this global crisis, but trying to fix everything everywhere comes at a cost of over 30 billion dollars a year, and it is unlikely that such funds can be mobilised.
Copenhagen Consensus [the author of this piece is the founder of the think tank], supported by funding from Merck for Mothers, worked with leading maternal health experts to use cost-benefit analysis to find the most cost-effective policies first.
The research focused on the highest-burden 59 countries that account for 91pc of all maternal deaths globally. Using the recognised Lives Saved Tool (LiST) model from Johns Hopkins Bloomberg School of Public Health, the researchers analysed more than 30 different ways to help and found that while all would have an impact, some would help much more for every dollar spent.
Two interventions stood out as the very best investments for additional resources. These are straight-forward without requiring cutting edge technology, but perhaps that is exactly why they are not well-known, lack celebrity endorsements and lose out on media coverage.
To drive the greatest impact for investments, the world should consider focusing on what is known as Basic Emergency Obstetric & Newborn Care (BEmONC) along with family planning. An estimated 217 million women who want to avoid pregnancy still do not have access to safe and effective family planning methods. Scaling up access to 90pc in the 59 countries would mean that fewer women would become pregnant, avoiding 87,000 mothers dying every year.
Getting more mothers into more facilities while also improving the quality of those facilities could help them and their children survive at a greater rate. In practice, this means ensuring that adequately trained staff are present with the right equipment and medicines to deliver simple and well-known life-saving procedures. These include immediate drying and thermal protection of the newborn, controlled cord traction, skin-to-skin contact of newborns, assisted vaginal delivery along with neonatal resuscitation.
All of this will entail costs. Midwives and nurses have to be educated, recruited and salaried; management expanded; drugs procured; and infrastructure paid for. Moreover, women also have to be incentivised to give birth in facilities. But overall, BEmONC and family planning would cost just 2.9 billion dollars a year — less than a tenth of the 30 billion-plus dollars typically asked for, which would save only a fraction more lives.
It would protect the women we have already promised to save at a very low cost: in total it would safeguard 162,000 mothers every year along with 1.2 million newborns. If we measure the total value of these efforts, each dollar spent would achieve 71 dollars of social benefits, making it one of the best investments in the world.
While a reader goes through this article, at least one more mother will have died. We owe it to her and all the millions whose lives we can save to invest 2.9 billion dollars smartly to bring hundreds of billions of dollars of economic and health benefits to people around the world.
PUBLISHED ON
Dec 26,2020 [ VOL
21 , NO
1078]


Agenda | Jan 30,2021

Fortune News | Feb 16,2019

My Opinion | Oct 09,2021

Editorial | Jan 18,2020

Fortune News | Jan 01,2023

Photo Gallery | 178141 Views | May 06,2019

Photo Gallery | 168351 Views | Apr 26,2019

Photo Gallery | 159120 Views | Oct 06,2021

My Opinion | 137050 Views | Aug 14,2021
Commentaries | Oct 25,2025

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Oct 25 , 2025
The regulatory machinery is on overdrive. In only two years, no fewer than 35 new pro...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Oct 25 , 2025 . By YITBAREK GETACHEW
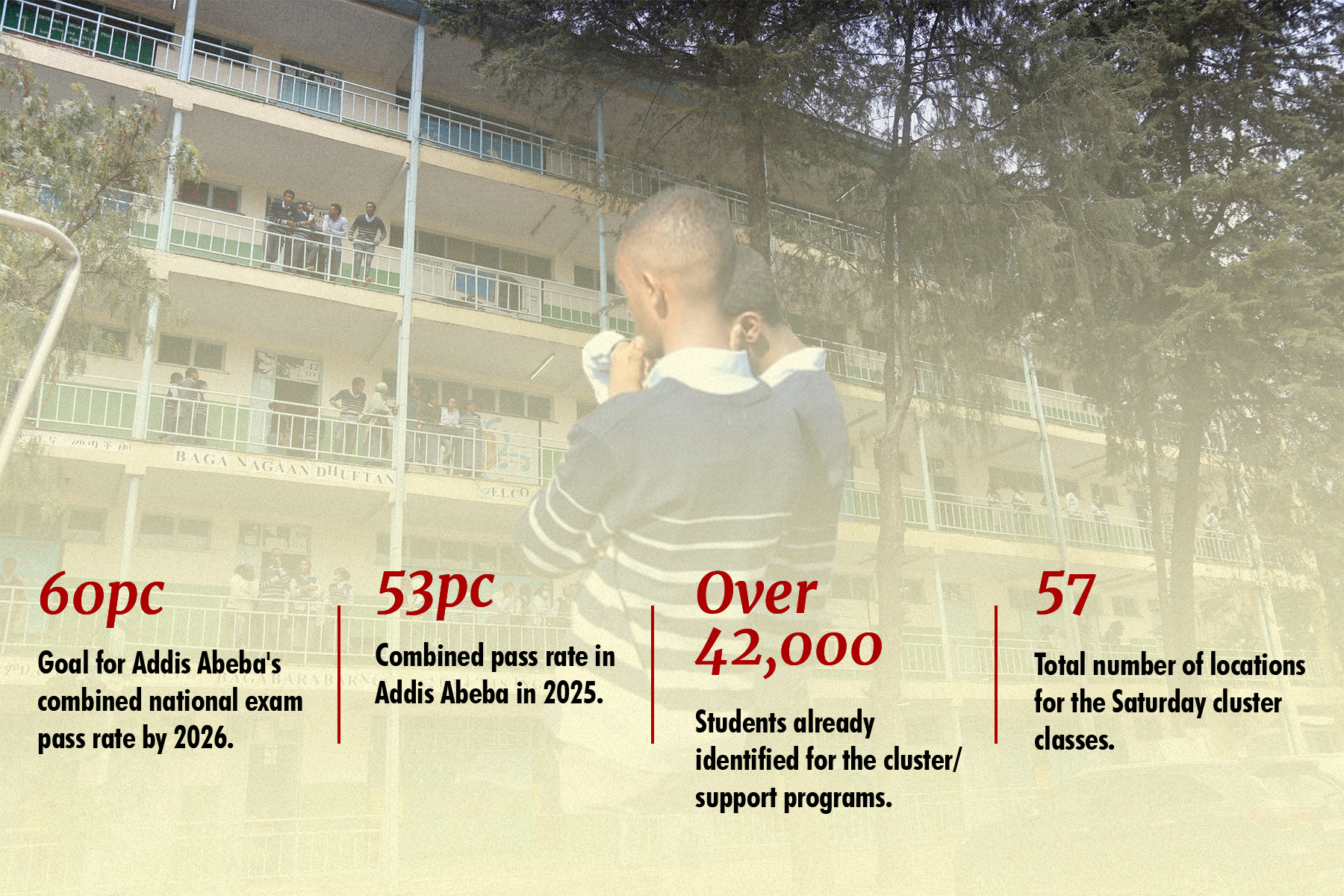
Officials of the Addis Abeba's Education Bureau have embarked on an ambitious experim...

Oct 26 , 2025 . By YITBAREK GETACHEW
The federal government is making a landmark shift in its investment incentive regime...

Oct 27 , 2025
The National Bank of Ethiopia (NBE) is preparing to issue a directive that will funda...

Oct 26 , 2025 . By SURAFEL MULUGETA
A community of booksellers shadowing the Ethiopian National Theatre has been jolted b...