
Sep 18 , 2021
By Halima Abate (MD)
Healthcare is expensive. Different factors fuel costs, including rising incidence of chronic conditions, lifestyle choices, increased aging population, liability concerns, obsolete technology and efforts by the healthcare providers to improve profitability. The matter is no different in Ethiopia.
Recently, the Ministry of Health has put in place a fee rate revision payable for medical services provided by the public hospitals. These health cost rises make the healthcare spending for the government painful, and tradeoffs are inevitable such as reducing spending on education or charging citizens more for out of pocket payments. This will have far-ranging consequences as health systems result from a complex mixture of institutions, regulations, conventions, and historical accidents.
Practical considerations often force decision-makers to deviate from the decisions they would make if faced only with the simple efficiency–equity maximisation problem. They have to consider political priorities and institutional constraints. Patients should normally pay the actual unit cost of services for under- or overutilisation not to occur. But there are always difficulties involved in tracking and allocating administrative overhead and other indirect costs to identify the true unit cost of health services.
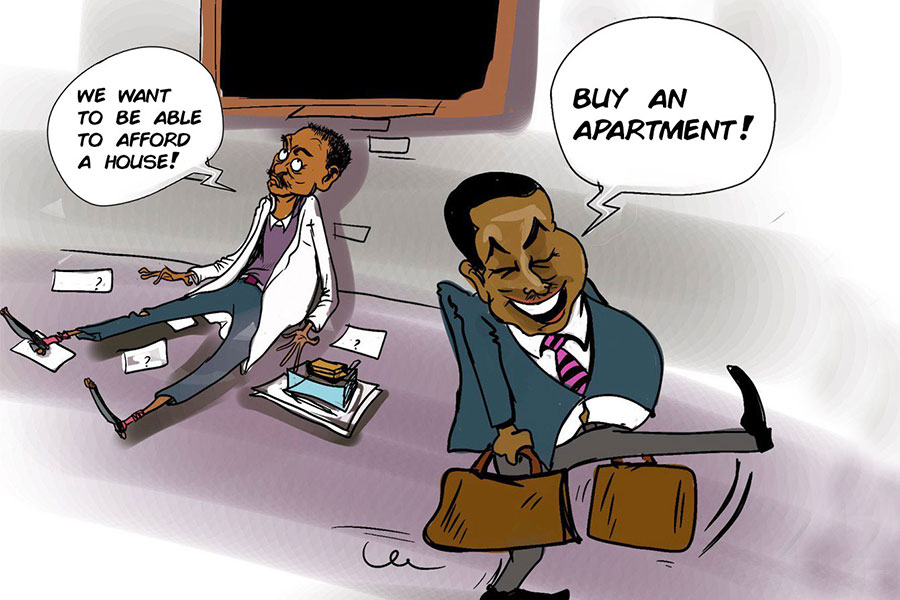
For those with low incomes, and thus less likely to have health insurance, out-of-pocket spending is the norm. It makes health care unaffordable and inhibits their ability to access care where needed.
None of this takes away from the importance of healthcare nonetheless, which is still critical whether or not people can afford it.
Healthcare is regarded as a basic human need by most people. Accessing health and confronting disease challenges requires action across a range of activities in the health system. Enabling access to healthcare paves a way to obtain health and health-related services with the following three components: physical accessibility (availability of health services with reasonable reach); financial affordability (people’s ability to pay for services without financial hardship), and acceptability (willingness to seek services). Access ultimately ensures universal health coverage, defined as the obtainment of preventive, curative and rehabilitative health and health-related services without incurring financial damage. Though access to health care does not guarantee good health, without such access, health is certain to suffer.
Hence, making improvements in the policy-making and stewardship role of governments; obtaining better access to human resources, drugs, medical equipment, and consumables; and encouraging a greater and deeper engagement of both public and private health care providers of services are crucial.
Great progress has been made in recent years within the health sector of Ethiopia for better access and to secure financial protection. This has contributed to improve not only health outcomes but also educational attainment, poverty alleviation and labour market productivity.
However, although healthcare should be a priority, without clear spending policies and effective payment mechanisms, the poor and other disadvantaged groups often get left out. Unfortunately, patients needs are often not translated into public policies.
Ministries of health such as our own, with respect to raising revenues for their health systems, explain how decisions on revenue-raising policy have an impact on universal health coverage. This is further undermined by international agencies that have been reducing financial support as a result of the recent downward trend in their own resources. Thus, a stable flow of funds to the health sector is critical to avoid disruptions in service delivery. Ensuring funds are raised in the most efficient way is also an important consideration.
Affording healthcare is a priority for both the insured and uninsured people. Beyond this, all health insurance systems have mechanisms for collecting and pooling revenues, spreading risk, and purchasing health services. Organising health insurance system with equity, efficiency and organisation in mind is fundamental in health care delivery system.
Through progressive financing arrangements, such as insurance systems, the government can subsidise the costs of health care for low-income individuals. The concept of national health insurance rests on the beliefs that everyone should contribute to finance health care and everyone benefits.
Yet progress is possible on a variety of fronts. This is particularly true in the area of e-procurement, which can make procedures more transparent, promote higher levels of participation, make it easier to track down anomalies, and generate data more efficiently. There is a clear need for further work to examine what methods are most effective in expanding access to essential care among the poor.
The proliferation of community-based health insurance schemes theoretically offers a way of addressing demand-side barriers into the benefit package. Yet, only one of the recent reviews of community schemes mentions that those costs cover a broad range of benefits which interact with existing health care programs.
The government should re-think its priorities to serve all income groups with the proper allocation of health service budgets instead of merely hiking prices.
PUBLISHED ON
Sep 18,2021 [ VOL
22 , NO
1116]

Films Review | Jan 25,2020

Viewpoints | Jun 29,2019

Viewpoints | Feb 01,2019

Fineline | Jul 27,2019

Films Review | Sep 10,2022

Life Matters | Jun 01,2019

Featured | Sep 10,2021

Sunday with Eden | Aug 16,2020

Sunday with Eden | Oct 23,2021

Viewpoints | Jun 12,2021

My Opinion | 131659 Views | Aug 14,2021

My Opinion | 128023 Views | Aug 21,2021

My Opinion | 125986 Views | Sep 10,2021

My Opinion | 123610 Views | Aug 07,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Jun 28 , 2025
Meseret Damtie, the assertive auditor general, has never been shy about naming names...

Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...

Jun 14 , 2025
Yet again, the Horn of Africa is bracing for trouble. A region already frayed by wars...
Jun 7 , 2025
Few promises shine brighter in Addis Abeba than the pledge of a roof for every family...

Jun 29 , 2025
Addis Abeba's first rains have coincided with a sweeping rise in private school tuition, prompting the city's education...

Jun 29 , 2025 . By BEZAWIT HULUAGER
Central Bank Governor Mamo Mihretu claimed a bold reconfiguration of monetary policy...

Jun 29 , 2025 . By BEZAWIT HULUAGER
The federal government is betting on a sweeping overhaul of the driver licensing regi...

Jun 29 , 2025 . By NAHOM AYELE
Gadaa Bank has listed 1.2 million shares on the Ethiopian Securities Exchange (ESX),...