
Viewpoints | Dec 26,2020
May 27 , 2023
By Natalia Kanem
In 2020, an estimated 287,000 women died in pregnancy, childbirth, or soon after delivering, according to the latest data from the United Nations Maternal Mortality Estimation Inter-Agency Group, which includes the United Nations Population Fund (UNFPA). This figure is roughly equivalent to the death toll of the 2004 Indian Ocean tsunami or the 2010 earthquake in Haiti, two of the deadliest natural disasters in modern history.
Human devastation on this scale is usually met with weeks of news coverage, an outpouring of public support, and calls for urgent action. Yet the staggering number of women dying every year in the act of giving life remains largely a silent crisis. Even more worrying, the group found that progress on reducing maternal deaths has ground to a halt.
How many of us know someone who died or came close to dying during pregnancy or childbirth?
Perhaps the pervasiveness of suffering is part of the problem – maternal deaths may seem inevitable. Yet the vast majority are preventable with simple interventions that save money in the long run.
One of the most cost-effective ways to reduce maternal mortality globally is to invest in community-based care, including educating and deploying midwives. Achieving this will require scaling up the workforce substantially – the world is currently facing a shortage of 900,000 midwives – and countering persistent gender norms that devalue the contributions of a predominantly female field.
Lowering the high number of unintended pregnancies is another crucial step toward reducing maternal mortality. UNFPA research shows that nearly half of all pregnancies are unintended, more than 60pc of unintended pregnancies end in abortion, and an estimated 45pc of all abortions are unsafe, making them a leading cause of maternal death. Policymakers know how to address this issue: increase access to quality contraceptives, improve comprehensive sexuality education, and protect women's right to decide whether, when, and with whom to have children.
World leaders have made significant progress when called upon to save women's lives. In 2000, governments agreed to the Millennium Development Goals (MDG), which aimed for a 75pc reduction in the global maternal mortality rate by 2015. The 44pc decrease in deaths over that period was a meaningful accomplishment – even if it ultimately fell short of the goal.
In 2015, with the UN's 17 Sustainable Development Goals (SDG), countries once again committed to reducing the maternal death ratio, this time to below 70 deaths per 100,000 live births by 2030. Yet, eight years on, we are nowhere near achieving that target, and progress has stalled.
The maternal mortality rate has increased in two regions – Europe and Northern America, and Latin America and the Caribbean – since 2016. These estimates, which end in 2020, do not account for the full impact of the COVID-19 pandemic on health systems.
Underinvestment in addressing persistent racial and ethnic disparities in maternal healthcare delivery contributes to this stagnation. In the United States, for example, the 2021 maternal mortality rate for Black women was 2.6 times the rate for non-Hispanic white women. Similar disparities can be observed in Afro-descendant communities in Latin America and the Caribbean.
A holistic, community-based approach to care is crucial to eliminating these disparities.
Early in my career, I worked as a pediatrician and HIV researcher in Harlem at a time when crack cocaine and AIDS were devastating the poorest and most marginalized patients and communities. It became clear that I could not treat a child without understanding the broader social context and the challenges facing the child's mother. And the medical needs of the mothers and pregnant women I met often paled compared to the urgency of their social needs, highlighting the importance of treating the whole person.
Even though progress on maternal mortality has stagnated globally, some glimmers of hope exist. Nepal, for example, decreased maternal deaths by nearly one-third between 2015 and 2020 after halving the country's rate between 2000 and 2015. In this period, the government doubled health spending, legalized abortion, and made maternity care free of charge.
Similarly, Sri Lanka has halved maternal deaths at least every 12 years since 1935, owing mainly to a health system that provides free services to the entire population and to a dramatic increase in the number of skilled midwives, who now attend 97pc of births, compared to 30pc in 1940.
While the latest maternal mortality rates reveal the damage caused by neglecting life-saving solutions, there is a way to end this needless suffering. Building midwifery capacity and ensuring equal access to quality sexual and reproductive healthcare would significantly improve health outcomes for mothers and pregnant women.
But getting back on track requires reviving the sense of urgency among governments, communities, and all stakeholders needed to provide adequate financing and create a conducive legal and social environment for these interventions. We know the reasons why women still die giving birth. Indifference should not be one of them.
PUBLISHED ON
May 27,2023 [ VOL
24 , NO
1204]


Photo Gallery | 178738 Views | May 06,2019

Photo Gallery | 168934 Views | Apr 26,2019

Photo Gallery | 159776 Views | Oct 06,2021

My Opinion | 137107 Views | Aug 14,2021
Commentaries | Oct 25,2025

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Oct 25 , 2025
The regulatory machinery is on overdrive. In only two years, no fewer than 35 new pro...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
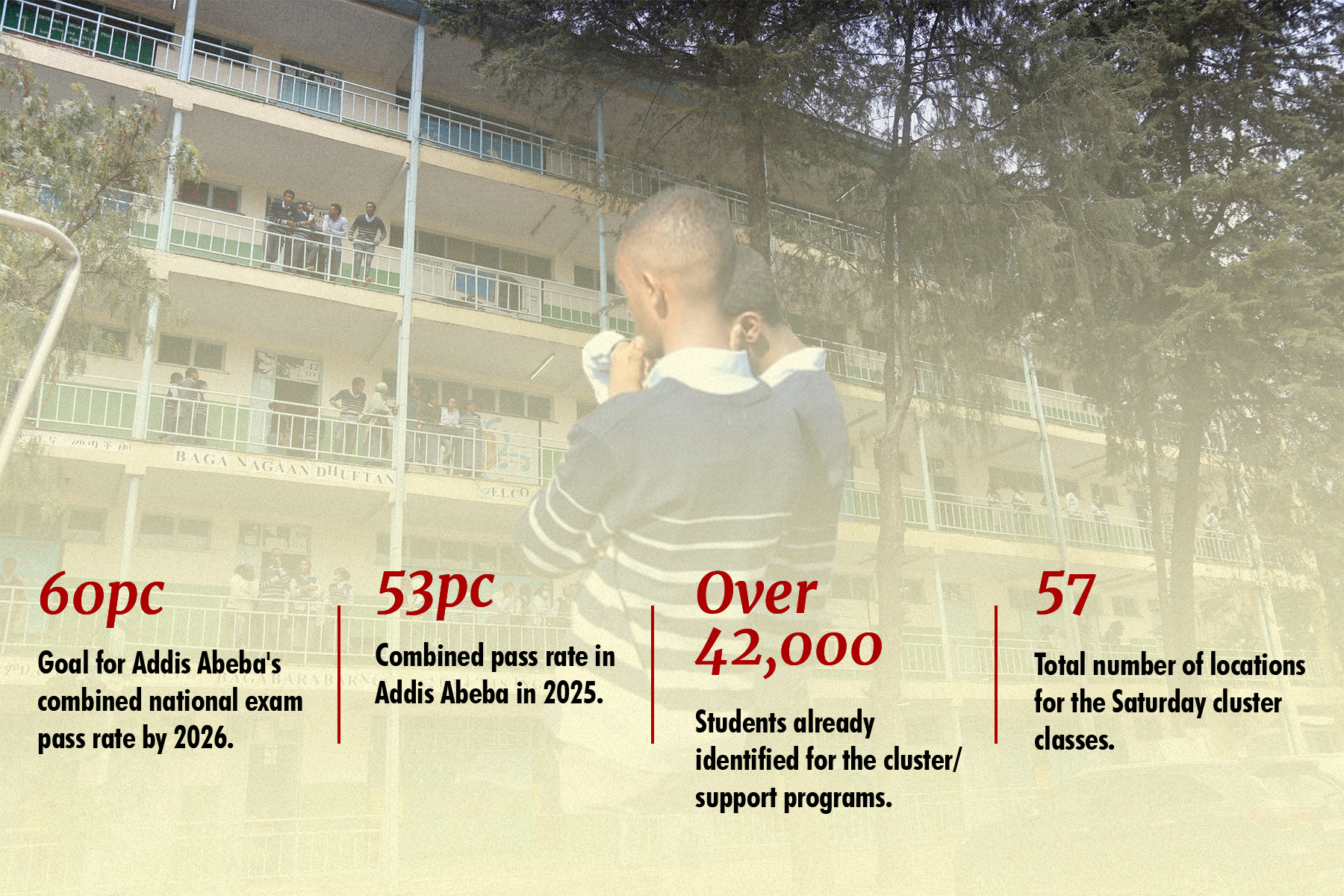
Oct 25 , 2025 . By YITBAREK GETACHEW
Officials of the Addis Abeba's Education Bureau have embarked on an ambitious experim...

Oct 26 , 2025 . By YITBAREK GETACHEW
The federal government is making a landmark shift in its investment incentive regime...

Oct 29 , 2025 . By NAHOM AYELE
The National Bank of Ethiopia (NBE) is preparing to issue a directive that will funda...

Oct 26 , 2025 . By SURAFEL MULUGETA
A community of booksellers shadowing the Ethiopian National Theatre has been jolted b...