
Fortune News | Feb 17,2024
A long-time diabetes patient, Almaz Teshome has been battling the effects of what she suspects to be substandard insulin bought from one of the pharmacies in public hospitals. Her condition worsened after using the medication, which she noted was visibly different from what she had used for 20 years. Her experience is part of a growing chorus of complaints from patients at Tikur Anbessa Specialized Hospital, who have reported that essential medicines, including insulin and chemotherapy drugs, have not been working effectively over the past year. Despite her reliance on community-based health insurance, Almaz is now considering buying medicine from private pharmacies, although the cost is prohibitively high.
The Ethiopian Diabetics Association (EDA) has acknowledged receiving complaints from patients about potential product defects but downplays the issue, suggesting that the problems might be due to improper administration rather than the medicine itself. However, recent research conducted by universities in Bahir Dar and Gonder reveals a troubling trend: nearly 22pc of medicine samples tested across sub-Saharan Africa failed quality tests. These medicines were found to be substandard, falsified, or unregistered, presenting serious risks to public health. The study uncovers the vulnerability of the pharmaceutical supply chain, which relies heavily on imports, with over 85pc of the market being met by foreign suppliers. India, the Netherlands, and Belgium are the largest sources, but the intricate and fragmented supply chains create opportunities for illicit products to enter the market. The Ethiopian Pharmaceuticals Supply Service (EPSS), the largest buyer of pharmaceutical products, has been urged to enhance its monitoring systems to ensure the safety and effectiveness of the medicines distributed to public health institutions.
While the Ethiopian Food & Drug Authority (EFDA) regulates medicine quality, it has received few official complaints, reflecting broader weak reporting and oversight issues. The EFDA has screened thousands of importers and disposed of millions of Birr worth of unauthorised or substandard medicines, but gaps in monitoring and reporting persist. Hospitals, including Tikur Anbessa, have been slow to submit adverse drug reaction reports, raising concerns about the effectiveness of the current pharmacovigilance system. The consequences of substandard and falsified medicines are severe, contributing to the rise of drug-resistant strains and undermining the effectiveness of legitimate treatments. This increases costs for patients and damages the reputation of the healthcare system. Despite efforts by local manufacturers like Addis Pharmaceutical Factory to maintain quality standards, the industry faces constraints, including forex shortages and the high cost of compliance with international standards.
PUBLISHED ON
Aug 11,2024 [ VOL
25 , NO
1267]

Fortune News | Feb 17,2024

Year In Review | Sep 07,2025

In-Picture | Jul 28,2024

Sponsored Contents | Jun 15,2022

Fortune News | Jun 01,2019

Fortune News | Sep 03,2022

Fortune News | May 27,2023

Fortune News | Oct 22,2022

Commentaries | Oct 26,2024

Radar | Jun 08,2025

Dec 22 , 2024 . By TIZITA SHEWAFERAW
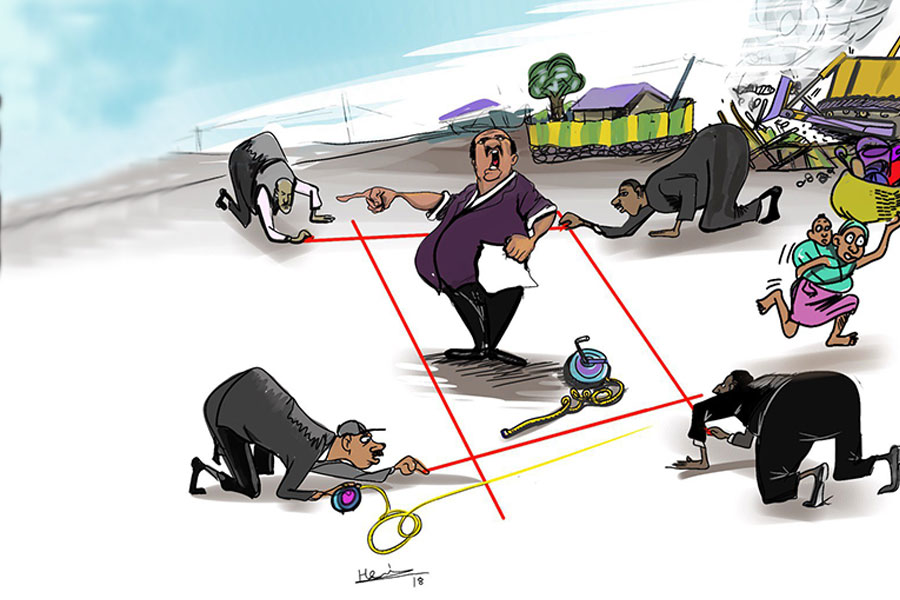
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
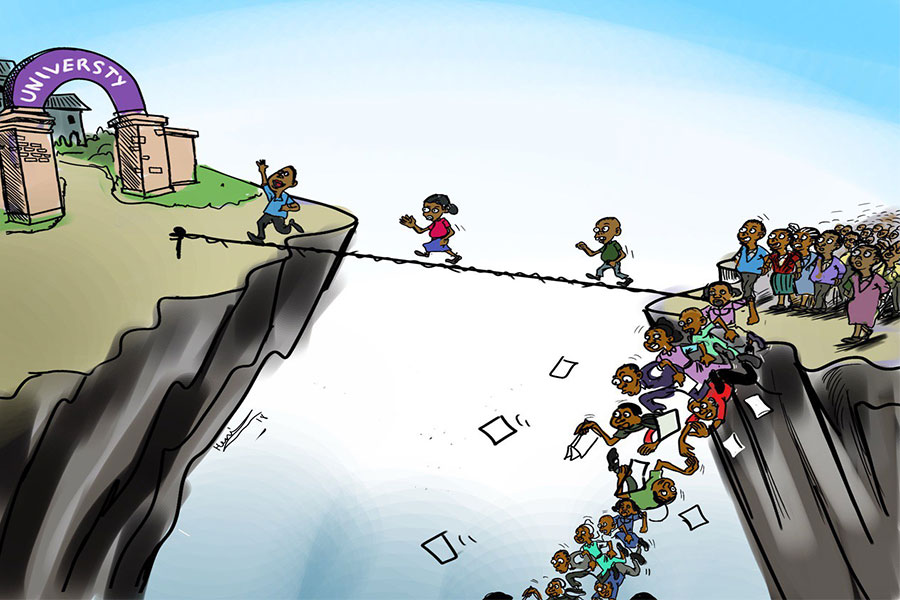
Four years into an experiment with “shock therapy” in education, the national moo...
Sep 20 , 2025
Getachew Reda's return to the national stage was always going to stir attention. Once...
Sep 13 , 2025
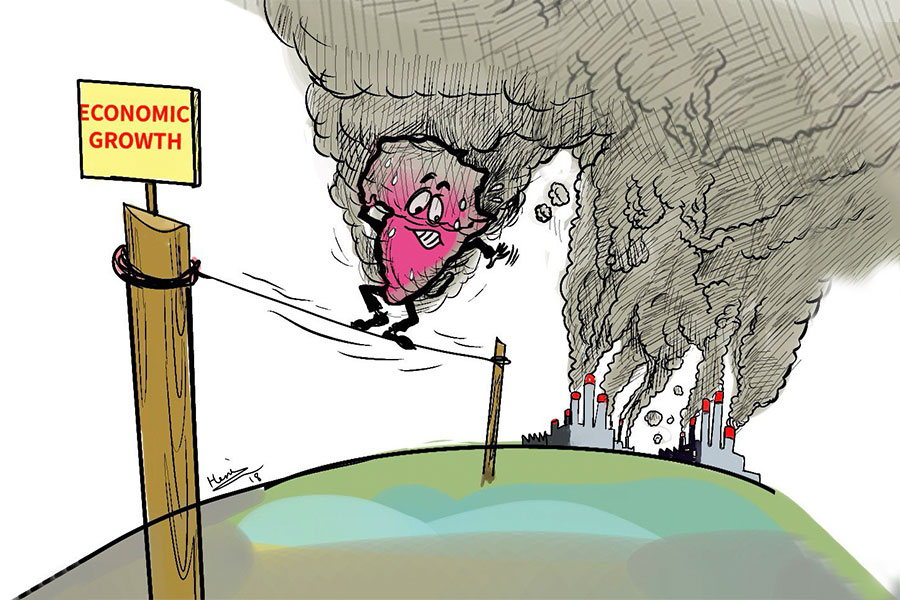
At its launch in Nairobi two years ago, the Africa Climate Summit was billed as the f...