
Commentaries | Sep 14,2024
Apr 11 , 2020
By Dawit Wondimagegn
Health care professionals are living in an unprecedented time. The responsibility of caring for patients while also maintaining our own wellbeing is pushing us into a corner.
Even though we knew all along that health care is a risky business, the threat of disease has never been this dramatic or widespread. The simple fact that being a health care professional is a risk factor for death from COVID-19 is scaring the life out of many of us. But under these circumstances, it is okay not to be okay.
We as a group will be going through a rough patch of physical, social and psychological experiences. In the early days of this epidemic in our country, the unknown is showering us with huge levels of anticipatory anxiety.
Epidemics force states and health systems to plan in a hurry. This means that there is limited or no opportunity for staff or stakeholders to contribute their share of input. This creates a lot of unknowns and uncertainties fueling more fear and anxiety among all.
This, of course, tends to be worse in a bureaucratic culture where participatory platforms are not a tool, and early and proper planning is not customary. All our past indulgences and indifference is catching up with us now. This haste and lack of opportunity for participation forces health professionals at the grassroots to feel less prepared to deal with the epidemic on the one hand and opens the state and health systems for influence by abstract forces on social media and individual exploitation, eroding an already dwindling public trust.
The creation of platforms for participation at a facility level, through the continuous supply of information, incident management sessions and training sessions is said to improve staff preparedness. However, the same needs to happen at higher levels of the system so that people at the grassroots do not continue to feel that they are being taken for granted and remain disconnected.
When the epidemic moves to a more active stage, health professionals will respond with a huge sense of patriotism and heroics as a result of the need to rise to the challenge. They will start to function with a collective willingness to work across strongly protected professional boundaries. All the attempts to push tasks across disciplines will disappear.
This will instead result in frustrations and confusion as previously designed system processes are no more in use, and the new order takes time to sink in. During this time, staff will respond by instinct. They will make mistakes as they do not have the headspace to consider all options in an unfamiliar environment with new people, a new disease and systems.
Health care professionals like it when they feel that they are in control. During the epidemic, as we start to see things we have not seen before, we lose the usual boundaries of working hours. All our social norms of sitting together and sharing a meal will be forgotten. Our work-life relationship will be tense as our family life becomes unsettled. There will be conflict between and within groups over a lack of agreement on what is urgent and what is not.
Leadership is central to mitigate such developments. The challenge for leadership, including myself, in this stage stems from simply focusing on getting things done. However, this leads to poor communication and silos of work stations where the chain of command is broken. Creating trust, confidence and reliance in lower level leaders such as department heads through distributive leadership is the way to move ahead.
Our leadership of this situation then demands that, in these early days of the epidemic, we make sure that we engage as many staff as possible in our thinking processes, establish a regular means of communication and, most importantly, avoid erratic patterns of communication that add to the chaos.
It is also important to use existing channels and structures instead of creating multiple parallel channels and, worse, multiple individual relationships, which is never a good idea anyway. There should also be a degree of transparency in terms of clarifying who is doing what. When staff understand what is happening, a feeling of calm and purpose will prevail.
As the epidemic progresses into a more advanced stage, staff will constantly be in full swing. They will almost fall into an "autopilot mode" and focus on what they do every minute. Unfortunately, this will lead to extreme self-neglect and exhaustion, as self-care will not be a priority. They will start to have problems at home as well.
Despite all this, healthcare workers will endure. The hardest thing they will struggle to cope with is going to be the moral distress they will have to shoulder. As resources get more and more scarce, healthcare professionals will be forced to play a mini-god, deciding who lives and who dies. This is in direct conflict with both professional and personal ethical codes. Of all the burdens that health professionals carry, moral distress will be the harshest. The disillusionment will be so intolerable for most that some may start to cope in harmful ways.
This is where both the public and the powers that be need to pay a lot of attention. The public can play a major role in reducing this potential burden by sticking to all the public health measures of intervention that are being implemented.
The math is clear. The fewer people get sick, the lesser burden to healthcare professionals. Health professionals themselves could play a much larger role in the early stages by engaging in a personal mission of public education and advocacy. We can prevent significant death, suffering and avoid the moral distress lurking on the horizon.
The powers that be have the ultimate responsibility of taking the measures that will ease the burden on health professionals. Primarily, their decisions must be made based on the weight of the available evidence. Resources should be allocated based on the evolving nature of the illness, not based on the usual rationing to satisfy other needs, including political ones. These are extraordinary times calling for extraordinary criteria.
We will eventually move to the end and recover from this epidemic. Nationally, there will be a heroes narrative. Everybody will claim some glory.
Health professionals will have the time to reflect. Most health professionals will come out of this with a profound sense of personal accomplishment. They will feel that they have coped successfully by using their personal, individual, community and organisational resources. They will experience personal growth after the trauma has passed.
This group will enjoy the heroes narrative the most. Other health professionals, however, will reflect on what they did and what they could have done differently, they may have some sense of shame and guilt - the heroes narrative will make it difficult for them to disclose their worries and problems. This will exacerbate their distress. Some will be changed by this experience. They will start to see their profession differently. Some may come to resent the individuals, organisations and the system they worked under.
It is in everyone's power to ensure health professionals will fall into the first category and come out of this situation feeling like heroes. So far, I have not seen enough attention being given to ensuring that health professionals are being taken care of. While the effort to get personal protective equipment from donors is laudable, there remains a need for institutional processes to be in place so that precious resources are used efficiently.
While the effort from many young people to contribute their share is promising, there are few structures that allow individual effort to be channeled into addressing one particular challenge.
For the goodwill and effort of many to bear fruit, we need to figure out a mechanism for cooperation and networking that leads to a defined goal.
Many artists are producing great, motivating pieces in the midst of this crisis. But their excellent work would have a greater impact if there was some kind of guidance so that the public will not get fatigued by boredom and repetition.
When all these efforts are coordinated in a cohesive manner, then health professionals will feel that they are being taken care of, and they will be okay not feeling okay. It is in your hands: wash them!
PUBLISHED ON
Apr 11,2020 [ VOL
21 , NO
1041]


Commentaries | Sep 14,2024

Radar | Jan 29,2022

Life Matters | Jul 18,2021

Radar | Feb 23,2019

Radar | Jun 11,2022
Fortune News | Feb 19,2022

Agenda | Nov 16,2024

Fortune News | Oct 21,2024

Viewpoints | Nov 05,2022

Agenda | Apr 30,2021

Photo Gallery | 174775 Views | May 06,2019

Photo Gallery | 164997 Views | Apr 26,2019

Photo Gallery | 155242 Views | Oct 06,2021

My Opinion | 136726 Views | Aug 14,2021
Editorial | Oct 11,2025

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
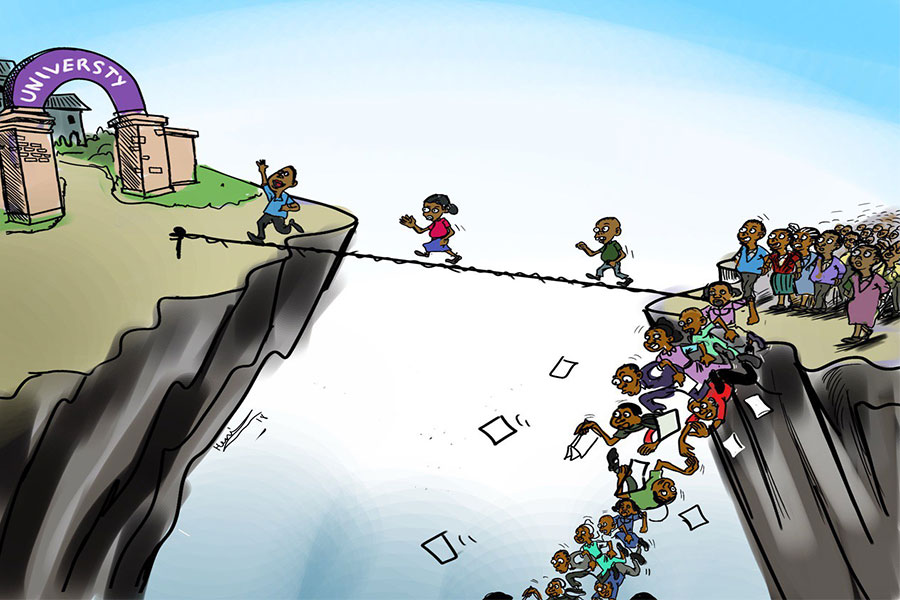
Four years into an experiment with “shock therapy” in education, the national moo...
Sep 20 , 2025
Getachew Reda's return to the national stage was always going to stir attention. Once...
Oct 12 , 2025
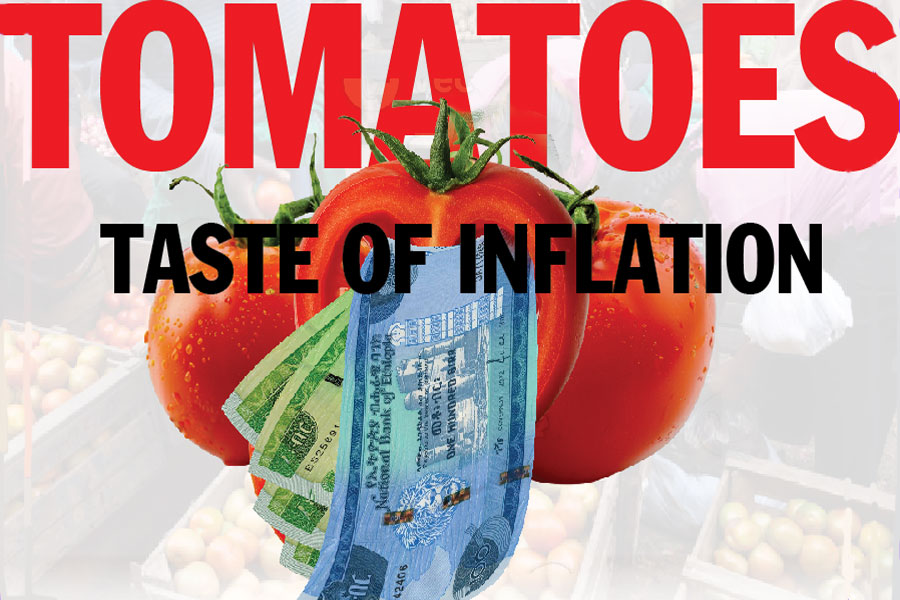
Tomato prices in Addis Abeba have surged to unprecedented levels, with retail stands charging between 85 Br and 140 Br a kilo, nearly triple...

Oct 12 , 2025 . By BEZAWIT HULUAGER
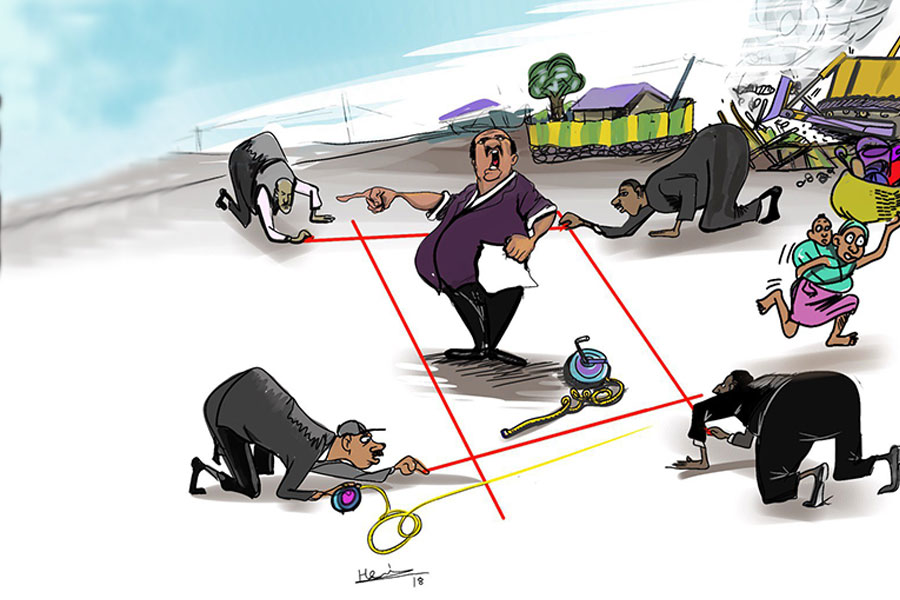
A sweeping change in the vehicle licensing system has tilted the scales in favour of electric vehicle (EV...

A simmering dispute between the legal profession and the federal government is nearing a breaking point,...

Oct 12 , 2025 . By NAHOM AYELE
A violent storm that ripped through the flower belt of Bishoftu (Debreziet), 45Km east of the capital, in...