
Verbatim | Jun 04,2022
Mar 27 , 2021
By Benji Pretorius (MD)
Impressive gains have been made in malaria reduction over the past 20 years. However, efforts to combat malaria must be accelerated if the disease is to be eradicated anytime soon. The fight against COVID-19 could provide a great lesson, writes Benji Pretorius (MD), founder of medical start-up ERADA Technology Alliance.
The World Health Organisation’s latest World Malaria Report provided great relief and hope to many. There is no doubt that globally we have come a long way in the fight against malaria over the past 20 years. Many countries have severely reduced the threat of malaria, with both Belize and Cabo Verde having reported zero indigenous cases in 2019 the first time in two decades. Additionally, both China and El Salvador have made a formal request for certification after a third consecutive year with zero indigenous malaria cases.
Within the last five years, seven countries have achieved a WHO certification of malaria-free status. The long road to worldwide eradication of malaria is shortening, step by step.
Yet 409,000 people still died from malaria in 2019, a preventable and treatable disease. Even as we celebrate incredible gains over the past 20 years and the millions of lives saved, the realities and immense scale of the scourge of malaria cannot be ignored. The global malaria death toll was estimated at 736,000 two decades ago; the reality we must face now is that 20 years of efforts worldwide to fight the disease has not even reduced the death toll by half.
This is not to sound pessimistic over what has already been achieved; it is important for the scale of the malaria burden and its consequences to be recognised globally if governments and world leaders are to understand that more action is needed quickly.
After the global COVID-19 pandemic, many more people across the world will understand the reality of living in fear of a largely preventable illness, fearing for friends and loved ones, and the inescapable awful reality that avoiding a potentially deadly illness often comes down to having some form of privileged status, job security, a decent income and, sometimes, simply luck. If the terrible COVID-19 virus has produced any positives, it would be that many more people will now understand the extreme importance of tackling diseases like malaria.
What can we learn from COVID-19 to help to eradicate malaria?
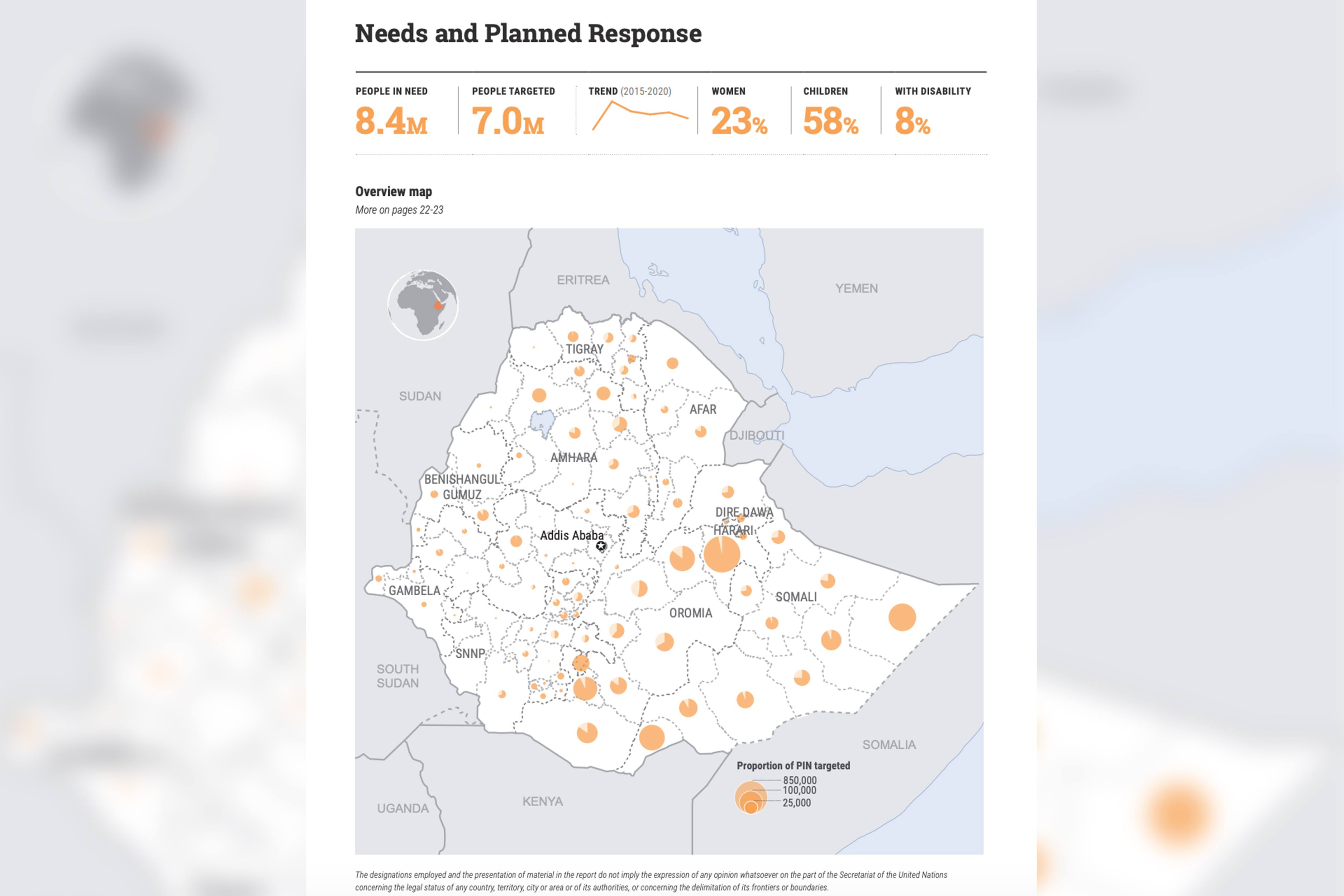
The COVID-19 pandemic revealed the need to invest in and expand healthcare systems across the world. The WHO African region, which bore 94pc of the malaria case burden in 2019 (an estimated 215 million cases), also has extremely fragile health systems that operate at near-capacity outside of a pandemic.
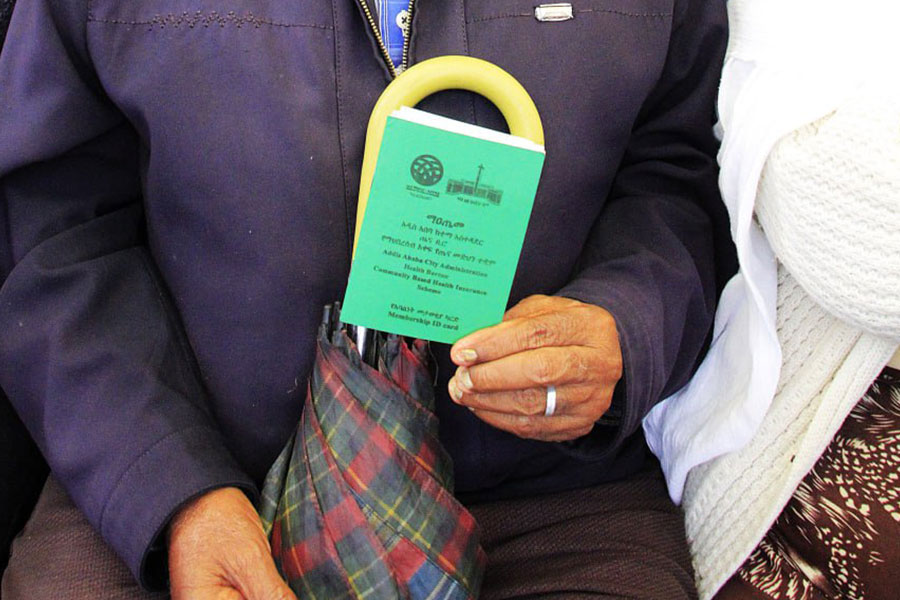
Accurate and timely rapid diagnostic tests (RDTs) for malaria that are simple to use and could be administered by the patient in their own home could help to ease the burden on strained health systems.
SALVA! RDT [a product produced by the company to which the author of the article is a managing director], which only requires children or adults to spit into a tube, delivers an accurate result in five to 20 minutes. It could be administered by parents, teachers or community leaders in homes or schools, taking the burden off medically trained professionals and allowing them to focus on treatment for malaria and COVID-19. There is no need to send samples back to a lab for testing, and for people who live in rural areas, a rapid diagnostic test like SALVA! could lessen reliance on health worker visits or having to travel a long distance to a clinic. In diagnosing and treating malaria, time is of the essence to give people the best chance of making a full recovery.
Around 2.7 billion RDTs for malaria were sold by manufacturers in the last decade, with an estimated four-fifths of these sold to sub-Saharan African countries, according to the latest World Malaria Report. Additionally, 1.9 billion RDTs were distributed by national malaria programmes during this time, with 84pc in Sub-Saharan Africa.
This is remarkable progress, but the distribution of RDTs is only part of the solution to combatting malaria. Greater access to diagnostic tools must be combined with strengthened and fairer healthcare models. The COVID-19 pandemic has further highlighted the danger of discriminatory healthcare models, where access to quality healthcare and life-saving medicines is more of a privilege than a human right. It is hard to imagine an end to the pervasiveness of preventable diseases in the world’s poorest communities when paying for medicine to treat malaria (less than 10 dollars) still pushes struggling families into debt. Tackling diseases like malaria, which disproportionally affects the world’s poorest, relies on improving access to affordable quality healthcare, as much as the distribution and availability of RDTs. Receiving treatment for an often deadly disease like malaria should not be determined by available income.
The fight against malaria is also a fight against poverty. The possibility of eradicating malaria within our lifetime depends upon accelerated and focused efforts to tackle both the disease and the level of poverty in the world’s poorest communities.
The world has changed dramatically since the start of the COVID-19 pandemic. Efforts to combat the novel virus have proven that governments and world leaders can come together to prevent loss of life on a grand scale. In rebuilding the new world, we now have the choice of what kind we wish to create.
It will be challenging, but possible, to create a world where the most vulnerable no longer die from preventable and treatable diseases and where everyone has access to quality healthcare regardless of income. However, it will not happen unless the world now comes together to demand more action to tackle malaria, with the same amount of focus, effort and investment that has been provided to tackle COVID-19.
PUBLISHED ON
Mar 27,2021 [ VOL
21 , NO
1091]


Verbatim | Jun 04,2022

Radar | Mar 23,2019

Life Matters | Sep 19,2020

Radar | Apr 24,2021

My Opinion | Jun 15,2024

Viewpoints | Oct 02,2021
Fortune News | Mar 13,2020

Covid-19 | Apr 01,2020

Viewpoints | Oct 23,2021

Fortune News | Nov 13,2021

Photo Gallery | 174822 Views | May 06,2019

Photo Gallery | 165043 Views | Apr 26,2019

Photo Gallery | 155299 Views | Oct 06,2021

My Opinion | 136727 Views | Aug 14,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
Four years into an experiment with “shock therapy” in education, the national moo...
Oct 18 , 2025 . By NAHOM AYELE
In a sweeping reform that upends nearly a decade of uniform health insurance contribu...

Oct 18 , 2025 . By BEZAWIT HULUAGER
A bill that could transform the nutritional state sits in a limbo, even as the countr...

Oct 18 , 2025 . By SURAFEL MULUGETA
A long-planned directive to curb carbon emissions from fossil-fuel-powered vehicles h...

Oct 18 , 2025 . By BEZAWIT HULUAGER
Transaction advisors working with companies that hold over a quarter of a billion Bir...