
Fortune News | Jul 08,2023
An Oncology centre inside the premises of Saint Paul Millennium Medical College is afoot as a French consultant finishes a feasibility study for the Public Private Partnership (PPP).
Under Abebe Gerbrehiwot, experts at the PPP Directorate Office, are currently reviewing the study conducted by a team of consultants from the Expertise Francaise for the past two years financed by the French government.
The Directorate functions under the Ministry, accountable to a nine-member board chaired by Minister of Finance Ahmed Shide and mandated to approve projects, including feasibility studies and major amendments to project agreements, as well as approving bids and negotiation outcomes.
It comprises Alemu Sime, Minister of Transport & Logistics; Mamo Mihretu, Governor of the National Bank of Ethiopia; Habtamu Itefa (PhD), Minister of Water & Energy; Chaltu Sani, Minister of Urban & infrastructure; Fitsum Assefa (PhD), Minister of Planning & Development, Binalf Andualem, Minister of Peace and private sector represented by Ethiopian Chamber of Commerce & Sectoral Association.
The Board’s venture into health comes four years after a law that governs public-private partnerships – the first of its kind – was legislated by Parliament. It came following a two-year feasibility study backed by the government, the African Development Bank (AfDB), and the United Kingdom’s Department for International Development (DfID).
Officials hope the scheme can fill a wide investment gap in the health sector.
Saint Paul Medical College is poised for the budget appropriation of 1.8 billion Br for the current fiscal year. According to Sisay Sirgu (MD), head of the medical college, the move aims to improve the college's human resources and financial models.
He said the private sector participation would seal gaps observed in service and medicine accessibility to patients and the provision of skilled human resources. The officials estimate that it will take up to 10 years for a return on investment and another 10 years for profit.
According to Abebe, a huge investment is required with an estimated initial capital of nearly 28 million dollars while annual operational costs take up to 20 million dollars. He indicated that they are trying to figure out the risk-sharing mechanisms between the private sector and government and the balance between financial profit and public service.
"It's too large and too complex," he said.
He said they plan to partner with developers such as the African Development Bank (AfDB) which will participate in giving transaction advisory services, finding funders and preparing tender documents once the board has approved the feasibility study.
Erected on 6,800sqm land, the nine-storey oncology centre will comprise nearly 340 beds, having the capacity to treat up to half a million patients annually. It is comprised of six surgical rooms, and radiation and nuclear energy treatments and can provide chemotherapy to 500 patients on a weekly basis.
Even though the oncology centre construction was slated to end in September, the rise in the cost of raw materials due to inflation pushed it till the end of January. The cost is predicted to be slashed when half the patients receive medical services through community-based Health Insurance while 10pc will receive medical care through premiums and 40pc in private.
Officials hope the public-private scheme can fill a wide investment gap in the health sector.
Two more constructions are undertaken on the premise; a cardiac center on 1400sqm and an organ transplant centre on 1900sqm with a 2.3 billion Br budget by the Ministry of Finance.
The public-private venture into the health sector comes following unsuccessful attempts at attracting investment in the energy sector. Abebe recalled that the absence of mechanisms that allow investors to underrate risk had caused the retraction.
Cancer incidences are increasing with nearly 72,000 new cases emerging on a yearly basis and over 60pc discovered after it surpasses the first stages. It accounts for seven percent of the total deaths making it the second most fatal after cardiovascular diseases. In 2030, estimates from WHO show that it would be the first killer disease in the country.
There were only three cancer health professionals and one treatment centre. Addressing the severity, the Ministry of Health penned a Cancer Control Program in 2013, a strategic plan that aims to increase oncologists, expand treatment centre facilities in major parts of the cities, and prevention methods.
Currently, the number of professionals has grown to 42 while treatment centres have grown to six, including Awassa, Mekele, Gondor and Haromaya.
In 2016, an oncology centre construction commenced at Paulos University, funded by the Ministry of Finance. Its absence prompts practitioners to write off patients to other hospitals.
Abdu Adem (MD), assistant professor of Clinicology Oncology at the hospital, said that up to 1,000 cancer patients make their way to the hospital on a monthly basis. His department has the capacity to take on 10 patients on a daily basis. With only 21 beds and limited medical supplies, the steady influx of patients has subjected patients to wait up to a month to get treatments.
Nearly 6,000 estimated cancer patients blust to the doors of the hospital waiting for cancer surgical operations, with only 22 operational tables under three rooms.
Mathiows Wondu Ethiopian Cancer Society is a non-profit organization that has worked on advocacy and support for cancer patients since 2004. It is currently supporting 172 patients.
Natnael Almeayehu (MD), an oncologist at the society, expressed optimistic sentiment proposed modality as he believes it will improve accessibility and timeliness of medical care to patients. He indicated the alarming increase in patients, the limited number of health professionals, and the shortage of medical supplies. He also indicated that patients are prompted to move abroad to take care of cancer treatments.
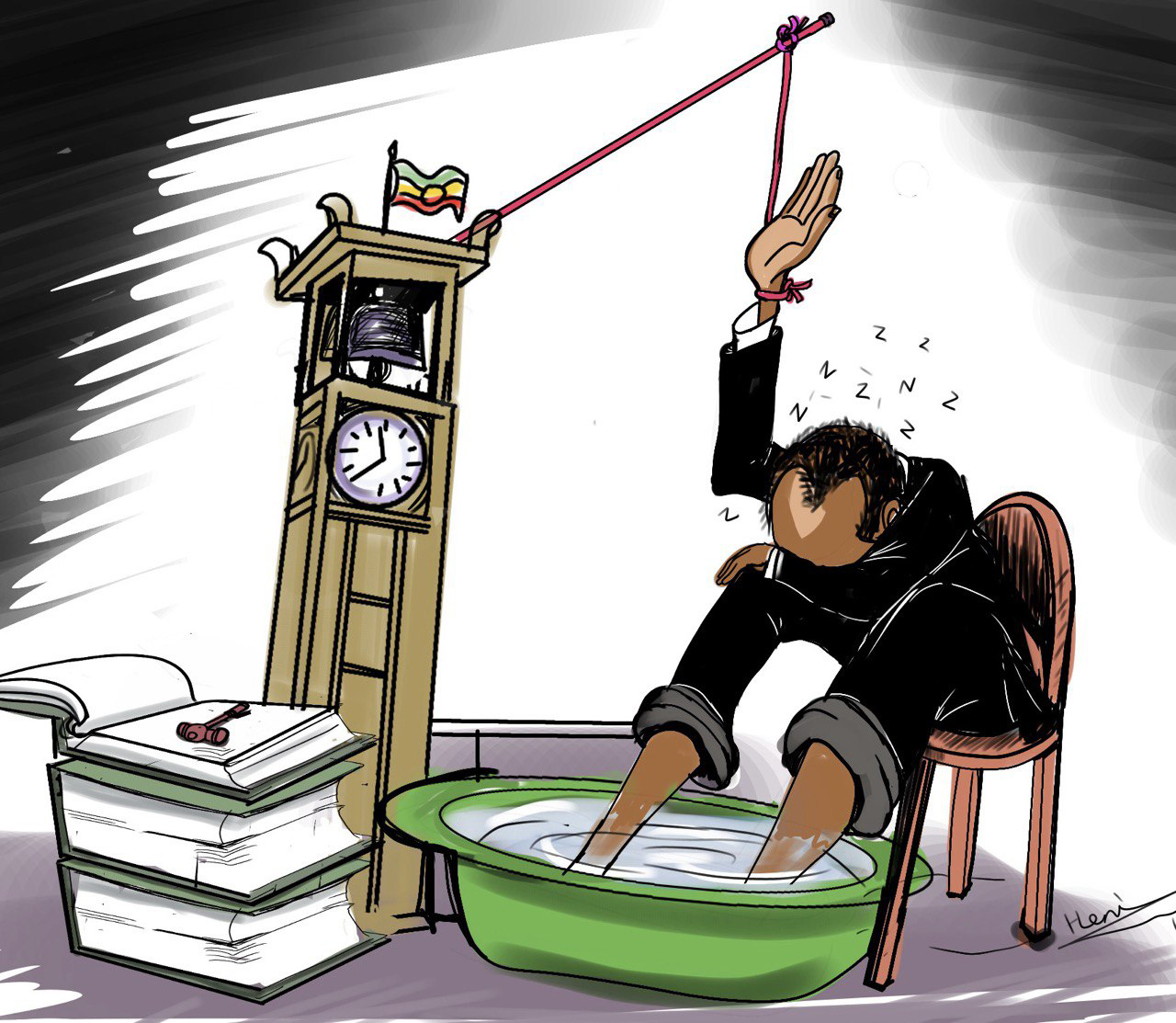
Getasew Amare, a health economist, said that public-private partnerships have been one of the ten policy pillars in public health services, which financial woes have savagely hit. He applauded the officials for paving the way to include them. He also recounted the success stories of many countries. He argues that even though the PPP scheme is viable as a strategy, he questions the ideality implementation. "Implementation is rather not that easy," he said.
He suggested that the PPP scheme be given proper care and effective management.
"It requires dedicated leadership and unrelenting oversight," he said. He suggested that the government should pave a smooth way for the private sector to remit profits for long-term sustainability.
PUBLISHED ON
Sep 16,2023 [ VOL
24 , NO
1220]

Fortune News | Jul 08,2023

Fortune News | Oct 13,2024

Fortune News | Jan 07,2023

Agenda | Jul 11,2021

Radar | Feb 04,2023

Fortune News | Nov 21,2018

View From Arada | May 03,2025

Radar | Oct 01,2022

Fortune News | Sep 10,2023

Fortune News | Apr 15,2023

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Jul 12 , 2025
Political leaders and their policy advisors often promise great leaps forward, yet th...

Jul 5 , 2025
Six years ago, Ethiopia was the darling of international liberal commentators. A year...

Jun 28 , 2025
Meseret Damtie, the assertive auditor general, has never been shy about naming names...

Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...