
For Abel Temesgen, 24, an incident that took place at Jimma University Specialised Hospital a month ago was one in a long line of abuses the medical field has been inflicting on practitioners.
The incident saw a female intern beaten up by an angry father that had just lost his daughter. This would serve to exasperate an already tense working environment that medical practitioners face in the line of duty.
This was not the perception Abel had of the medical field. The first child of his family, his interest in the human body led him to the medical field.
Graduating with high grades from high school, he became one of 375 students to join medical school in Addis Abeba University’s Class of 2013.
“Med school was no walk in the park,” he says. “We had a very short time to prepare for exams. We're busy all the time.”
Dropouts, nervous breakdowns and cry outs were common. Their final year, they say was worse, when they had to endure internships.
“Tikur Anbessa Hospital [Black Lion] is an overcrowded old hospital that lacks basic medical facilities and continuously fails to help its patients,” says Abel.
This is a sentiment shared by other intern students around the country. A major source of discontent for the interns is the long working hours coupled with a low salary and benefits. Interns work for 36 straight hours two times a week on average, while they are paid 3,600 Br a month.
“Additionally, the interns also had doubts over their future and job security,” says Abel.
Around 450 graduate doctors placed at different regional health centres were forced to return after the facilities informed them that there was no budget to employ them.
The interns also asked for risk allowance, saying that they risk being affected by contagious diseases in their professions.
As the medical interns’ demands received wider traction, Prime Minister Abiy Ahmed (PhD) held discussions with 3,000 health professionals, students and private organisations and associations on May 4, 2019.
It was during this period of rising frustration that the Jimma incident took place.
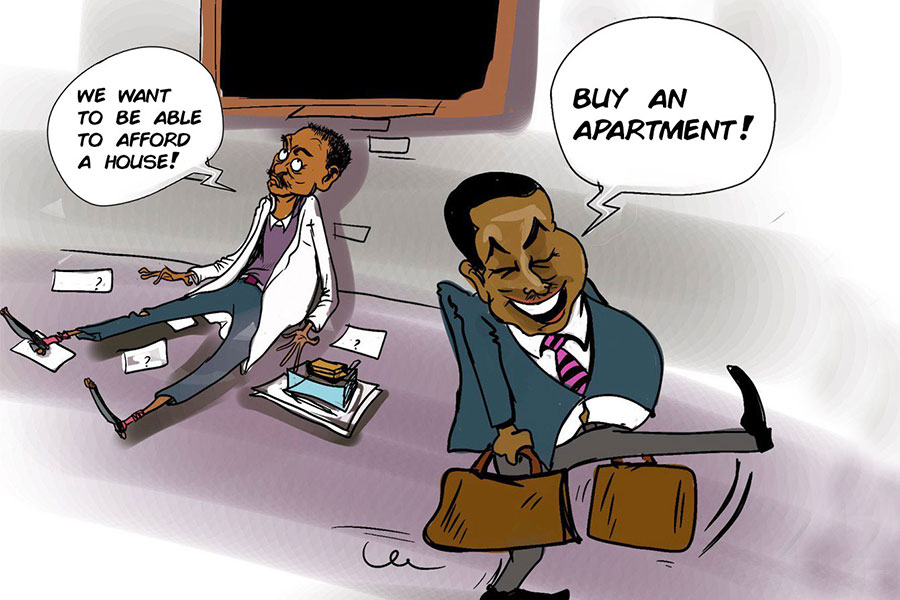
Interns at the University reacted to the incident with a strike demanding better working conditions, a reduction of working hours, better pay and improvement of medical facilities. These demands were picked up by interns in Arsi University’s College of Medicine & Health Science, and a demonstration was held.
Following a forceful response by the police in Arsi, interns at Meqelle, Gonder, Addis Abeba, Dire Dawa and Adama University brought up similar demands, some also participating in strikes.
“The demands are not raised for any self-serving or financial reasons. They are minimum requirements for a properly functioning health system,” stated a letter written by the interns at Adama University's Medicine College.
The strike has taken on country-wide importance, drawing other practitioners across the country to the issue.
“Aside from the countless problems the health care system is facing nationwide, very old operating rooms with non-functional and outdated equipment, poor sterilising materials, on-and-off working autoclave machines, unsanitary recovery rooms, and overwhelming infection rates have been serious challenges,” reads a statement from Gonder University Surgery Residents.
While other sectors have been changing, the health sector has remained stagnant, according to Berhanu Nega (MD), vice president of the Ethiopian Medical Association.
“The myriad of problems in the health sector are the result of neglect by the government,” Abraham Araya (MD), a resident physician at St. Peter Hospital in the capital. Abraham is the founder of a social media page, Hakim, that supports and provides a platform for the striking interns.
“The government only allocates three percent of GDP to the health sector,” added Abraham.
There are nine doctors for every 100,000 people in Ethiopia. In low-income countries, there is an average of 30 doctors for every 100,000. With 400 hospitals in the country, there are only 9,182 doctors, 16,765 nurses and 1,379 midwives.
Despite the low numbers, the medical field has shown significant improvements over the past decades. The Ethiopian government has been successful in maintaining its polio-free status since January 2014, when the last case was reported in Somali Regional State.
Health Minister Amir Aman (MD) stated that the Ministry recognises the problems but added that the students should be more patient. This is an opinion shared by experts who cite that the interns are still civil servants.
Considerable efforts have also been made to improve the expansion of health infrastructure. For instance, the number of functional health posts, health centres and hospitals in the country has sharply increased by 16pc, 33pc and 108pc in the first half of this decade, according to a report by UNICEF.
Mortality rates for infants and those under five years of age have more than halved, and life expectancy has been raised to an average of 65 years from just 47 years in 1990.
Nonetheless, medical practitioners claim that there is a great deal of work to be done.
Medical service is hellish in Ethiopia, and it has always been doctors that suffered the brunt of the criticism, according to Abraham.
“We see patients sleeping on the floor and dying as there are no rooms available,” says Abenezer Tarkegn, an intern at Black Lion Hospital. “We feel terrible, but we learned the hard way to walk away, as we couldn’t do anything, and the society ended up perceiving us as the bad guys.”
Considering the traction the issue has received soon after the protests, efforts have been made to tackle the problem, including holding public discussions.
One of these was a meeting with Prime Minister Abiy Ahmed (PhD) and 3,000 health professionals, students and private organisations and associations on May 4, 2019. Health policy, the medical and health education system, health insurance and salary and benefits were central talking points.
The Prime Minister addressed the gathering by noting the government’s effort at medical tourism. Changes in the procurement procedure for the importation of pharmaceuticals, setting up of pharmaceutical industries, the allocation of 120 million dollars for the purchase of medicine and the development of 4,200 housing units in 340 health centres throughout the country were cited as progress throughout the past year.
“Demands of the sector should be lodged with respect to the current socio-economic status of the country,” the Prime Minister added.
The attendees of the meeting did not appreciate the Prime Minister’s answers.
“He not only failed to address our questions but was misinformed about our profession,” says Abraham, who was also one of the attendees.
Almost all 269 interns at Black Lion Hospital undertook a strike beginning last Monday. This was despite the Ministry of Health announcing several changes to be introduced to the health sector on the same day.
These include a reduction of university fees for medical students from 470,000 Br, which was introduced to hold graduate students to two years of service, to the regular cost-sharing scheme.
The budget was also allocated for the employment of 3,800 specialised doctors in different regions and hospitals.
“We are working on the administrative and system hurdles that could be addressed immediately, but most of the problems in the health sector need patience and time,” Amir Aman (MD), minister of Health, said at a press briefing on May 10, 2019.
A joint task force composed of officials from universities at every medical college and the Minister of Higher Education & Science has been formed to investigate the issue and come up with a recommendation within a week, according to the Minister.
The Minister, while acknowledging the problems, does not believe that such strikes will be productive. This is a sentiment shared by Gemechu Ararssa (PhD), lecturer in the field of Public Administration & Management at Addis Abeba University.
“While their questions are legitimate, they shouldn't hold medical service as a hostage,” he said. “They are civil servants and should think of the public at large.”
Interns like Abel disagree with this, seeing the strikes as the only option.
"They might postpone our graduation or fail to give us jobs,” said Abel, whose younger brother has followed in his footsteps. “But the hospital can’t function for long without its interns, and our demands will ultimately be met.”
Nonetheless, Abel admits that their strikes could be cause for institutional failures that can lead to human death and suffering.
“If our presence becomes necessary, we will cover the emergency room, newborn intensive care unit and delivery wards,” he said.
PUBLISHED ON
May 11,2019 [ VOL
20 , NO
993]

Life Matters | Apr 17,2020

Fortune News | Mar 27,2021

Viewpoints | Aug 27,2022

Fortune News | Jul 09,2022

Fortune News | Jun 05,2021

Viewpoints | Jan 09,2021

Fortune News | Mar 16,2019

Viewpoints | Jan 05,2019

Sunday with Eden | May 11,2019

Editorial | May 08,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Jun 28 , 2025
Meseret Damtie, the assertive auditor general, has never been shy about naming names...
Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...

Jun 14 , 2025
Yet again, the Horn of Africa is bracing for trouble. A region already frayed by wars...
Jun 7 , 2025
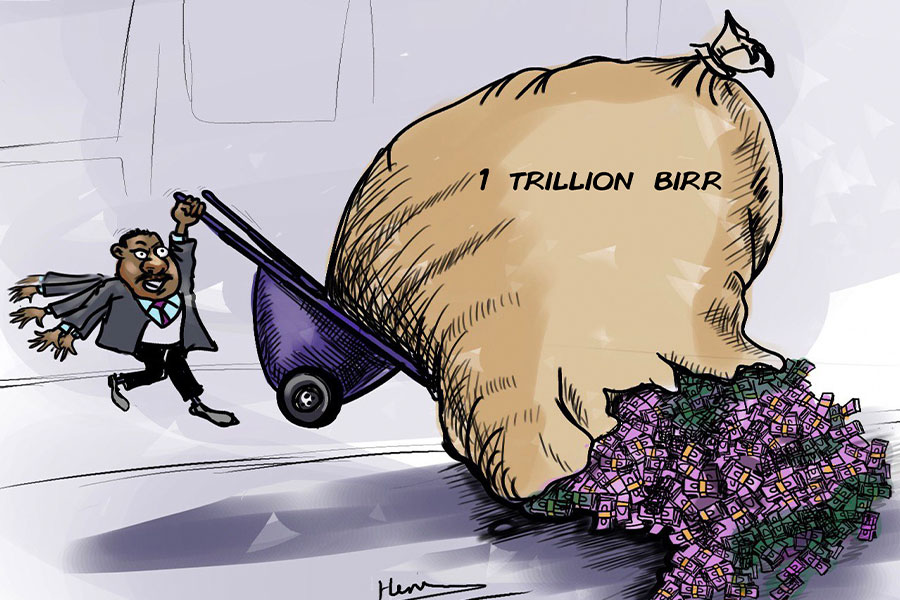
Few promises shine brighter in Addis Abeba than the pledge of a roof for every family...