Radar | May 16,2020
When Amanuel Hinsta (MD), 28, joined the Gonder University Medical School a decade ago, he was as hopeful as a young man with good grades can be. He envisioned a bright future with a prestigious career with financial security for a lifetime.
Five years into the stressful journey of medical school, the urge to drop out began prevailing as he observed the lives of his supervisors that had left him uninspired by what awaited him. Despite discontentment in the field, he managed to get to the finish line and secure a job at Zewditu Memorial Hospital as a general practitioner. The monthly net wage stands at 9,000 Br, which momentarily increased during the Covid-19 pandemic. However, Amanuel claims the year-and-a-half stint exposed him to "traumatising" working conditions while it failed to reimburse him financially.
Amanuel has found himself in a difficult situation where living costs have become overwhelming. As a result, he has decided to explore opportunities to relocate abroad. With a focus on Canada and Australia, he spends most of his time researching and applying for residency programs.
"I had to find another way," he told Fortune.
A national survey conducted in 2022 has shown that 32pc of the employed physicians have made plans to leave their medical occupation to other businesses by the following year, while 48pc are dissatisfied with their job.
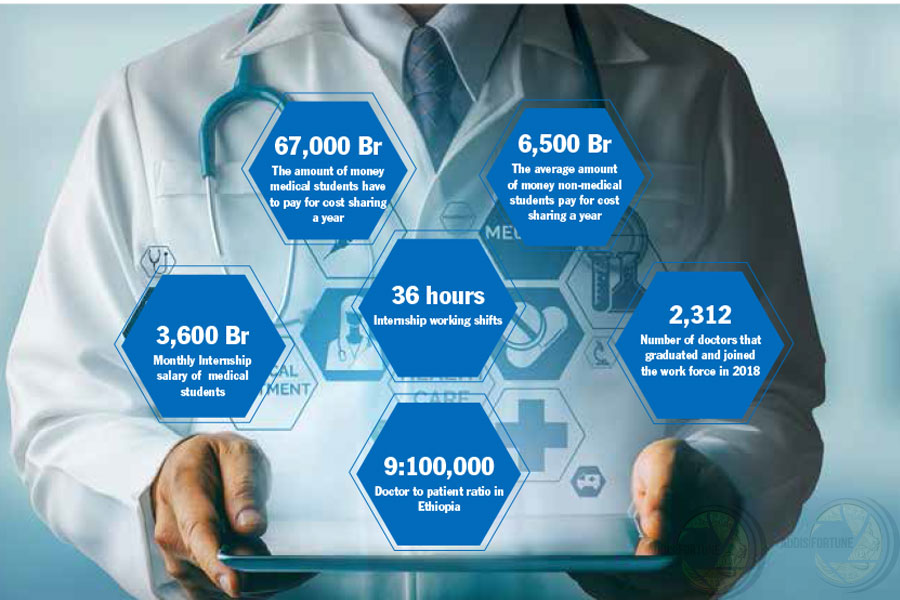
Low wages despite long working hours, dismal opportunities for advancing the educational status and flawed governance are the major impediments cited by medical doctors for such results. The prestige and financial security associated with being a physician have diminished through the years, with their monthly salary averaging around 400 dollars. The average annual salary of medical doctors in the US stands at around 165,366 dollars prompting physicians to opt to leave the country.
Ethiopia ranks top five in the continent in terms of medical brain drain despite having physicians (per 1,000 people) reported at 0.1 in 2020. The WHO median standard for health workforce density is 4.45 physicians for 1,000 people.
A study conducted at Addis Ababa University showed that around 53pc of medical graduates wanted to immigrate to the United States and Europe after finishing their studies.
Tegebar Yigzaw (MD) is the president of the Ethiopian Medical Association, with 5,000 members. He believes unemployment, a combined effect of outdated standards and the health centre's budget constraints, is the number one push factor forcing medical doctors out of the country.
"It's discouraging," he said.
Since 1987, close to 75pc of physicians fled the country within a couple of decades, in search of better prospects abroad.
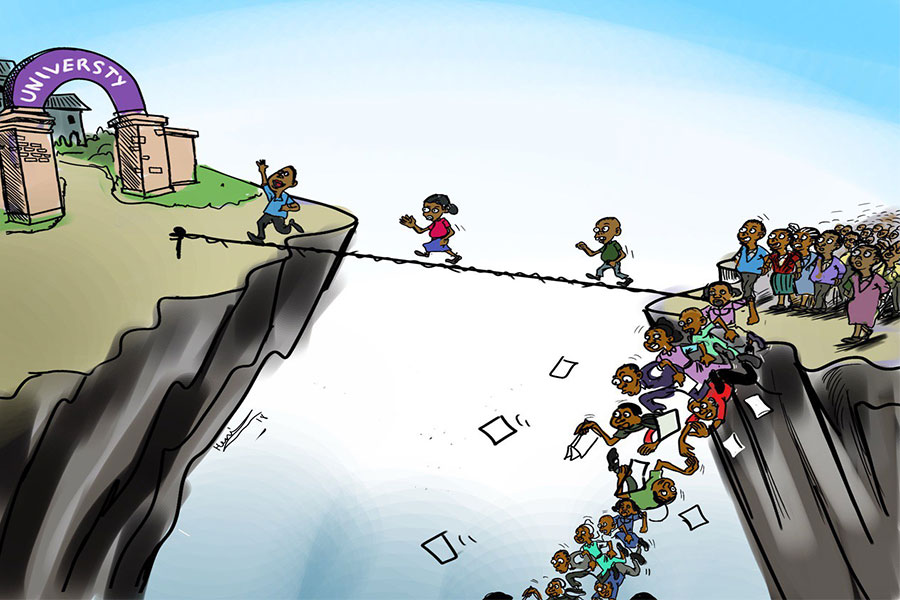
The policy that aimed at producing a flooding number of physicians practised by the Ministry of Health until 2019 led to a four-fold increase in the number of physicians lest a concurrent increment in hospitals capable of absorbing them.
Despite reduced enrollment to medical school by 2,300 students annually, half the size from six years ago, there is no fiscal capacity to accommodate the workforce. The Ministry is contemplating starting a matching fund to ease the burden on public hospitals by allocating 70pc for employing upcoming medical doctors.
"The health workforce production and the institutional capacity have not been going in tandem," said Assegid Samuel, head of Human Resources for Health Development & Improvement at the Ministry. He disclosed the Ministry is not against physician migration unless it affects the labour market in the country.
Assegid said they have eased the requirements for opening private practices and facilitated the necessary funds to open up offices while doubling the staffing capacity by revising the standards with hopes of mitigating unemployment.
"We have been working with credit associations," he said.
There are about 20,000 medical doctors, a stark shortage compared to a population above 100 million. In the meantime, the burden of unemployment has cast a shadow as the country's 353 public hospitals and 3,706 health centres grapple with limited budgets. To accommodate the large medical workforce, nearly 120,000 hospitals need to be built, as the 30pc absorption rate of the private sector is deemed small in comparison to the 20 medical schools.
Established in 1964, the state-owned Tikur Anbessa Hospital, the largest in the country, provides several treatments unavailable elsewhere, with a daily intake of above 15,000 patients. It has nearly 768 faculty members toiling around to serve thousands queueing up to get treatment.
Siraj Awol (MD), a third-year resident at the gynaecology department of the hospital, is tending to The bags under his eyes reveal that he had a sleepless night tending to nearly 30 patients. His 10,000 Br monthly salary barely covers his living cost, while the frustration fuels him up as he becomes unable to meet the demands of his patients due to limited medical supplies.
"I would leave the country if any opportunity opens up," he told Fortune.
The budget deficit has been a serious problem that has only worsened through the years. Under Addis Abeba University, Tikur Anbessa Specialised Hospital has a 400 million Br budget allocated for the year. The shortage of medical supplies is only getting worse, according to Demelash Gezaghegn (MD), emergency medical services director.
He observes the budget division for teaching and medical services diminishes its efficient allocation with credit supplies from Ethiopian Pharmaceutical Supply Agency (EPSA) unable to cover the need.
A mere three percent of the total 786.6 billion Br budget went to the health sector in 2022/23, amounting to 19 billion Br. Underpaid, overworked and psychologically stressed professionals with late overtime payments only serve to worsen their woes.
Andualem Deneke (PhD), president of Tikur Anbessa and vice president of Addis Ababa University, said that while pull factors like better pay and working conditions drove most doctors out in the past, prevailing economic constraints are now serving as push factors for physician migration.
"The budget covers only a fraction of what is really needed," he said. A series of reforms seeking to bring budgetary autonomy to Tikur Anbessa from the federal government is considered a promising development by Andualem.
Experts argue that a series of policy reforms are necessary to accommodate the workforce as significant funds have been invested in each graduate.
Getasew Amare, a health economist, argues that centralised political decision has prompted the health sector to be given one of the lowest investments with political interest that breeds high return rates. The absence of technology, monitoring and accrediting entities to health facilities, and the absence of an institution that plans based on long-term forecasts compound the problem, according to the health economist.
"Funds are diverted to other sectors," he said.
According to the expert, weak leadership has hampered financial resources, such as public funding, research grants, scholarships, and infrastructure investments. The practice of expecting foreign finance to plug in 30pc of the health sector budget has led it to be overlooked. He said the budget allocation has failed to comply with the floor set by the World Health Organization, which stands at five percent.
"It is inherently expected to sustain itself," he told fortune.
Getasew stresses the importance of those who are in leadership having bargaining power of convincing the importance of health investment. He advises policymakers to recognize the impact of low-quality health care and lack of access and appropriately allocate a budget.
PUBLISHED ON
Jun 17,2023 [ VOL
24 , NO
1207]
Radar | May 16,2020

Viewpoints | Oct 24,2020
Sunday with Eden | Oct 31,2020
Radar | May 25,2024

Commentaries | Oct 22,2022

Viewpoints | Dec 26,2020
Fortune News | May 11,2019

Radar | Apr 08,2024

Fortune News | Aug 11,2024

Radar | Oct 12,2025

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...
Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
Four years into an experiment with “shock therapy” in education, the national moo...