
Fortune News | Mar 19,2022
A 59-year-old man, an actor by profession, fell severely ill about five months ago. His son, Binyam, and his family took him to St. Yared Hospital to get him a check-up, unsure of what his illness might be. Doctors ordered a CT Scan and discovered that he had a pulmonary edema, the presence of excess fluid in the lungs. He was not at that point tested for the Novel Coronavirus (COVID-19), but the doctors had suspected that this could be the case.
To make matters more complicated, Binyam's father had pre-existing conditions of hypertension and diabetes. He was transferred to Ras Desta Damtew Hospital, where he had a subsequent follow-up. The doctors there also suspected that he had contracted COVID-19 but started treating him right away as his glucose levels were critically low. He remained oblivious to what was going on. Not wanting to worsen the situation, the medical staff were reluctant to tell him he had indeed contracted the deadly virus, Binyam recalled.
"They told us he had COVID once his glucose levels stabilised," said Binyam.
As his breathing was interrupted, his father was put on oxygen support for four days. Once his glucose levels were stable, he was moved to Semegnew Health Centre, an isolation facility then used by Ras Desta Hospital. He was kept on oxygen support for a couple of days more.
Binyam’s father was not the only one in the family to contract the virus; his mother, two sisters, and Binyam himself tested positive shortly after. The rest of the family managed to recover unharmed, with his mother struggling with mild symptoms for about two weeks. Ever since, the entire family makes it its purpose to stay as cautious as possible. Binyam continued working, being careful while his parents stayed at home, keeping outings to a minimum.
Unfortunately, the family’s tragic episode with COVID-19 continued after Binyam’s aunt, 65, contracted the virus. She was looked after at home and doing fine. Suddenly, about a week ago, it became difficult for her to breathe, and by the time she was taken to a hospital, it was too late. She died of the COVID-19 virus, which has so far claimed the lives of 2,900 people in Ethiopia. Globally, over 2.8 million people have lost their lives.
Binyam’s father is one of more than 159,000 people who were able to recover across Ethiopia.
The virus's spread has seen a sudden spike in recent months, indicating that Ethiopia indeed faces a third-wave since the first person with the virus was identified in March last year.
There were reactions in desperation, pushing parliament to declare a state of emergency on April 8, 2020. This week marks one year since the first six-month-long emergency law was decreed, restricting gatherings for religious, public, social or political purposes. Physical proximity, recreational outings, prison visits, face-to-face classes, and many more threats identified as risks for public health were constrained by law. The sixth national election was postponed indefinitely, only to be rescheduled to be held in about three months from now.
Many wonder now if the spread of COVID-19 was the real reason behind postponing the elections last year; the surge in new cases is at an all-time high now.
Although members of the public exhibited some resistance, early last year was when people, especially urbanites, adhered to preventive measures. The country swallowed its breath, waiting for the daily case updates released by the Ministry of Health (MoH) under Lia Tadesse (MD). A State Minister before the pandemic, she assumed the role of public-health-officer-in-chief, replacing Amir Aman (MD) shortly before the pandemic broke out.
Millenium Hall treatment centre, which used to accommodate up to 80 patients at once, started receiving 52 patients a day beginning in January. It now treats 220 patients at a time.
The daily cases then picked up from three to eight per week, while the number of critical cases was very low. The first death, which was received with great shock, was recorded on April 5, a couple of weeks after the first positive case in the country. To expand isolation and treatment centres, medical facilities, schools, hotels and halls were quickly transformed into hospital wards. In doing so, about 148 centres for tens of thousands of patients were made available throughout the country.
Later in early October 2020, all isolation centres were closed.
One of the makeshift centres was Millennium Hall, on Africa Avenue, near Bole International Airport. It remained open throughout. What served as a venue for festivities and public gatherings for over a decade was turned into a medical facility, initially a quarantine and a treatment centre for up to 700 people. Later, it was fully converted to a patient care centre with 140 beds, 19 intensive care units with ventilator support, and 20 high-dependency units for those in need of heavy amounts of oxygen.
Abel Mureja (MD), director of the centre, began to see cases spiking in late January 2021, a month when the centre had between 70 to 80 patients admitted. Supervised by St. Paul's Hospital, Abel leads a 400-strong medical staff at the Millennium Hall treatment centre; they all have received vaccinations as frontline workers meriting priority.
One of these frontline workers is Rediet Gebregziabher (MD), who had been serving her mandatory duty in Jijiga since 2017. She moved back to the capital to join in the fight against the pandemic in June 2020. Much like many frontline workers, Rediet had contracted the virus in December of last year. She isolated herself for two weeks and went back to work.
However, her test remained positive, a case some patients are faced with. Even though they have recovered and the disease is not communicable, some continue to test positive.
Her main engagement at Millennium Hall was facilitating testing for isolated patients. Rediet has noticed that the trend in infection has significantly changed even beyond the numbers. In the beginning, the demography of patients who sought critical care was the elderly, usually in their 80s. Lately, however, young people, some in their 30s, are admitted. The Millennium team started receiving 52 patients a day beginning in January, compelling the authorities to expand beds for 220 patients, with 32 ICU patients and 40 high-dependency patients. Despite the expansion, the centre remains fully occupied at all times.
"The patient flow has tripled since January," said Abel.
The month of March has arguably been the most challenging for the country since the pandemic broke out. Thirty deaths, the highest ever in a day, were recorded on March 13, 2021, while new cases showed a 150pc jump from the previous month. To make matters worse, a severe shortage of oxygen cylinders caused by a production disruption at Chora Gas Factory has created chaos combined with the overcrowding of critical care units.
Demand for medication and oxygen has also gone up. The centre used up to 250 cylinders of oxygen a day a few months ago, but the oxygen need has doubled since. The severe shortage of oxygen cylinders in Addis Abeba over the past few weeks has been offset as sources from Hawassa, Sululta, Bishoftu (Debre Zeit) and Addis Abeba mobilised to improve the situation. The shortage is similar to that of certain medications used to prevent blood clotting.
To accommodate the rising number of patients in need of critical care, St. Paul's Hospital has allocated an additional building with the capacity of 40 beds, equipped with oxygen supply and ICU, to complement the existing units that accommodate 14 patients. It has been a trying time for the frontline workers at St. Paul's, where four senior staff members lost their lives to COVID-19.
The Hospital, which ordinarily treats up to 2,000 patients, started admitting COVID-19 patients in early June; the daily requests range from 15 to 20 patients in need of critical care who are now denied admission as the centre is fully occupied.
"We think we're living through the worst of times," said Berhanetsehay Teklewold, director of inpatients at the Hospital.
It is such a subtle but unpronounced realisation of the pandemic's gravity that forced the authorities to allow private care providers to give COVID-19 treatment, although only late into the pandemic. No less than seven private hospitals – such as Hallelujah, Yerer and Bethezatha hospitals, as well as the American Medical Centre – are providing treatment for COVID-19, albeit at high costs.
The American Medical Centre, a private health centre founded in 2012, began to admit COVID-19 patients in December 2020 with two intensive care units and a specially designated ward for 10 patients. The Hospital is operating at capacity now, the Medical Director of the COVID-19 treatment unit, Tinsae Alemayehu (MD), told Fortune. He leads a team of up to 15 healthcare staff but faces shortages of medical equipment, much like the rest of the centres in the country.
"Everything is in short supply," Tinsae said.
A specialist in infectious disease, Tinsae believes COVID-19 will not easily go away even though people are getting the jabs, not unless the whole world is vaccinated and for all strains of the virus, according to him.
There are now close to 600 million people vaccinated globally, of which 1.7pc took full jabs, while 4.3pc have received at least one dose. This remains a fraction of the vaccines required by the global population.
The only semblance of good news in the midst of this chaos came a year down the road when the Ministry of Health started rolling out the AstraZeneca COVID-19 vaccine in mid-March after receiving 2.2 million doses donated through the COVAX facility, a UNICEF global initiative working toward equitable distribution of COVID-19 vaccinations.
This week, the Ministry has received another 300,000 doses of vaccines from China. Priority for vaccination was given to frontline workers, who are far more likely to contract the virus, and the elderly, who are prone to COVID-19-induced complications. However, many of the senior ministers and officials serving the administration of Prime Minister Abiy Ahmed (PhD) received vaccine shots in the United Arab Emirates two months ago, according to people familiar with the process.
The Ministry announced late last week that it had concluded the vaccination of medical professionals and has invited the elderly and those who have underlying health conditions, such as Binyam's father, to register beginning this week.
Rediet was one of the early recipients of the vaccine. She was one of the few people who had faith in the vaccine, with resistance and skepticism rife among the public. Even her parents were against the idea.
"Each called me and told me not to get vaccinated," she told Fortune.
She went ahead, however, in the hope of setting an example in addition to protecting herself. These vaccination brands arrived right around the time studies were released doubting the safety of the Indian-made vaccine, which did not help the situation. The case against the vaccine was founded on claims that it caused blood clotting.
Blood clotting is a common case in COVID-19 patients. But clotting caused by the vaccine as a side effect is a rarity. It is a much better scenario than the virus, argued Rediet. As more research supporting her conviction surfaced and through frequent nudges from those already vaccinated, more people started warming up to the idea though. With that, almost all of the staff have received vaccine doses.
The situation repeated itself in St. Paul's Hospital as well, where up to 70pc of the staff have been vaccinated. People let go of their fears as they saw those who got vaccinated were well, observed Berhane.
As cases seem to be surging, having faith in the provisions of vaccine supplies that cover only a fraction of the population can be fatalistic. Officials at the Ethiopian Public Health Institute and the Ministry of Health are struggling to reinforce preventive regulations, encourage home-based treatment and isolation, and enable private facilities to start COVID-19 treatment, according to Yehualaw Getahun, a public health specialist at the Ministry.
"Tough times are ahead of us," Yehualaw warns.
Those in the fight and the frontline call on the public to adhere to preventive measures, urging that these should come second nature to people.
"Prevention is the only way out," said Tinsae of the American Medical Centre.
Daily reports of the pandemic's death toll are seen as mere figures by the public, but for people like Binyam and many others on the receiving end of COVID-19, they are reminders of the loss of loved ones. A visit to one of the churches or burial places of other faiths speaks loudly that the pandemic is hardly over.
PUBLISHED ON
Apr 03,2021 [ VOL
22 , NO
1092]

Fortune News | Mar 19,2022

Radar | Sep 14,2019

Commentaries | Jan 15,2022
Editorial | Jun 04,2022

Editorial | Mar 14,2020

Fortune News | Mar 25,2023

My Opinion | Jul 31,2021

Radar | Apr 01,2024

Radar | Nov 14,2020

Fortune News | Aug 29,2020

Dec 22 , 2024 . By TIZITA SHEWAFERAW
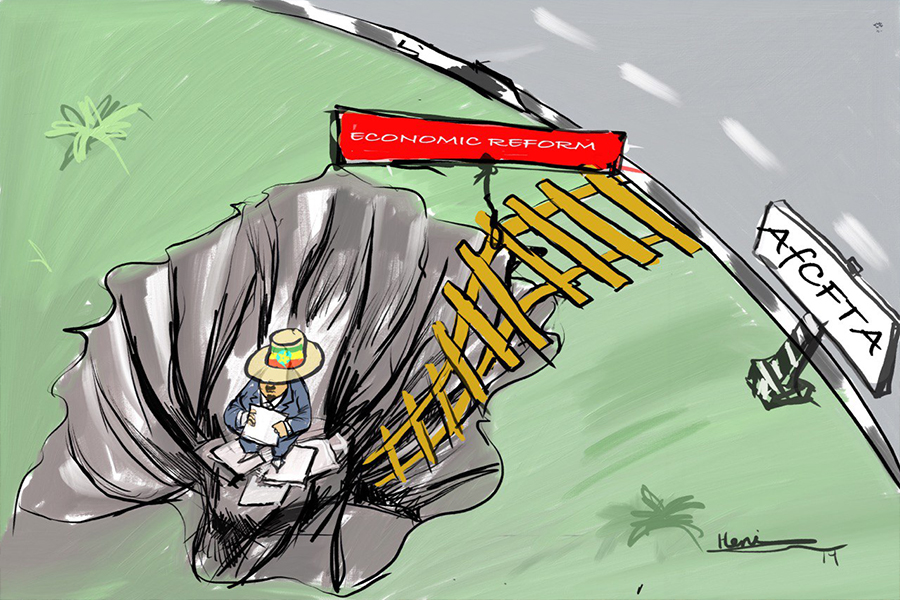
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Jun 28 , 2025
Meseret Damtie, the assertive auditor general, has never been shy about naming names...

Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...

Jun 14 , 2025
Yet again, the Horn of Africa is bracing for trouble. A region already frayed by wars...
Jun 7 , 2025
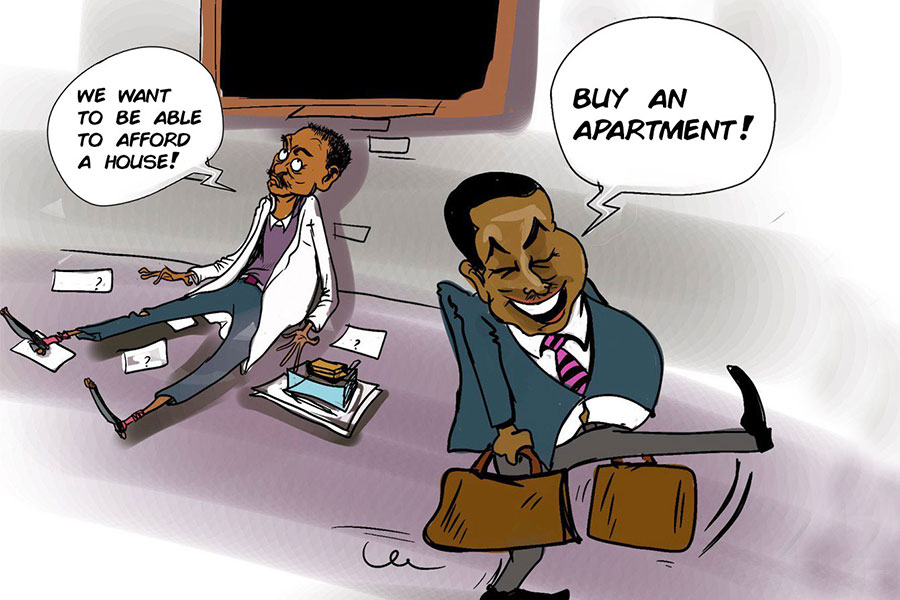
Few promises shine brighter in Addis Abeba than the pledge of a roof for every family...