
Radar | Jan 04,2020
Last month, a very unlikely Novel Coronavirus (COVID-19) patient walked through Yerer Hospital's halls. Yerer was the third private hospital licensed to provide treatment to the victims of the pandemic, a service that was previously limited to government-run hospitals and health centres in the country, though the new private options carry steep price tags that the average Ethiopian could hardly afford. The patient: a 60-year-old domestic worker.
Yerer, which is located in the Goro neighbourhood and has joined the ranks of Addis Abeba Silk Road and Hallelujah Hospital, was an option for those who were willing to pay for better care and attention than was provided at free government-run centres. The domestic worker, who wishes to remain anonymous, hails from a very modest background in the rural area of the country's northern region. Nearly 15 years ago, she came to the capital looking for work, and she found it in the domicile of a well-to-do family.
Over the years, she grew close with her employers, and their bond turned into one of family, a bond that would eventually help save her life. A family member in the house had tested positive a few days before she started showing symptoms herself. The illness would eventually require her to seek respiratory support, and the family took her to Yerer Hospital, where they paid an initial deposit of 90,000 Br. By the time she was discharged, 10 days of oxygen support, multiple laboratory tests, meals and other costs meant that the family had to top that up with an additional 30,000 Br.
Hers is one of the less shocking stories that would make the rounds in the city as people were reportedly discharged from private health centres with bills as high as 1.5 million Br. Initial deposits varied from one private health centre to another, ranging from 25,000 Br to nearly 300,000 Br.
Though intended to buffer and support the COVID-19 response, private healthcare providers' addition in the fight against the pandemic is turning out to be less altruistic than intended. The high bills come with an even longer list of justifications, primarily personal protective equipment (PPE), the cost of which is covered by the patient in care.
Face masks, face shields, hazmat suits and gloves are all tacked on to the bill upon discharge. Medication like Heparin, an anticoagulant prescribed for patients in critical condition, is valued at over 700 Br a pill while other commonly used ones are tallied around 300 Br. Risk pay for specialists like anesthesiologists, emergency specialists and internists is then added to the price tag, all before profit margins come into play.
At some hospitals like Addis Abeba Silk Road General Hospital, the costs run even higher as most staff live in a hotel to mitigate contagiousness, seeing as they provide around-the-clock COVID-19 healthcare. Silk Road, a Chinese-owned and operated hospital specialising in neurosurgery, was the first private COVID-19 treatment centre on the scene after signing a memorandum of understanding with the Ministry of Health to cater to high-end clientele such as diplomats.
The Hospital, built at a cost of 300 million dollars, originally opened its doors in November 2019 with acclamation from the then Minister of Health, Amir Aman (MD), who would leave his post a mere month before the pandemic dramatically altered healthcare both in the country and around the world.
In order to attend to needs arising from the pandemic, the Hospital shut down all other operations and dedicated its 100 beds to COVID-19 patients. Nearly 50 staff, physicians and nurses were relocated to stay at a nearby hotel, personal protective equipment was procured, and the Hospital even went as far as facilitating training and experience sharing by a team of Chinese doctors in April last year.
Its connections helped it source PPE relatively easier than other treatment centres. It provided disinfecting services to public health facilities and quarantine centres when they were still functional. Inadequate resources have since then forced the closure of all quarantine centres with only five public COVID-19 treatment centres still operating.
Hallelujah General Hospital, which provides services like dialysis treatments for kidney problems, was the second private healthcare institution licensed to provide COVID-19 treatment from the government.
But costs were running very high for the Hospital itself, which had left its expensive, state-of-the-art operating rooms and diagnostic machines idle, according to Ruth Eshetu, human resources & administration manager at Silk Road. To mitigate the expenses, it contracted beds out to the likes of the United Nations and the Chinese Embassy.
The Ministry of Health then put a manual in place to involve the private sector in the efforts against the pandemic, which had an ever-rising number of positive cases, and as a response to patients who had the financial means for levels of personal care the government could not provide.
With nearly half of healthcare in the country provided by the private sector, engagement in COVID-19 care was unavoidable. Recently, Bethzatha General Hospital and the American Medical Centre have been added to the private COVID-19 treatment centres, bringing the total number in Addis Abeba to five.
But regulating the private sector in this regard would prove to be tricky, according to Yakob Seman, head of medical services at the Ministry of Health.
"We wanted to create a sense of confidence in the general public first before opening [treatment] up to the private sector," he said. With that in mind, training private facilities and slowly initiating them into the process through the provision of free testing centres was started.
The manual was set in motion last August to set a standard method of operation and to regulate COVID-19 treatment at private health centres with directions set to limit prices for treatment. The reviews on the price caps, which were based on price assessments conducted throughout hospitals in the city, were mixed. But even as operations commenced following the guidelines, complaints flowed in from patients who believed they were unfairly charged.
"There were centres operating within the legal lines but that were using other means to make more money," explained Yakob.
Laboratory test prices may have been regulated, but the frequencies would be manipulated, as assessments carried out by the Ministry revealed later on.
"Instead of running one test, they'd do five or six," said Yakob. The manual's loopholes were not taken for granted.
But the support was still substantial, explained Yakob, as it provided alternative options for treatment and elevated the image of the country. The complaints coming to the Ministry were handled through stern letters so as not to discourage efforts.
Providing PPE and other necessary supplies for free to private healthcare centres was considered as a way to lower the costs, according to Yakob. But the proportion of public to private facilities in the country would make that plan hard to implement. Public hospitals providing COVID-19 treatment in the country contain over 90pc of the 2,500 beds available for patients; PPE and other supplies were in very high demand.
The global disruption had also affected the procurement of PPE. Contract cancellations, delays in arrival and other issues were an obstacle to the required amount reaching the country. Nonetheless, the Ethiopian Pharmaceuticals Supply Agency has recently disbursed a round of COVID-19 supplies, its ninth since the pandemic's onset.
This fiscal year, the Agency has distributed supplies, including nearly 300 mechanical ventilators, worth 1.7 billion Br. But officials at the Agency estimate this number to be higher as donations included in the supplies are calculated at much lower prices than market value. Despite this, security disruptions across the country had hindered the deliveries with road blockades delaying trucks carrying the supplies to the Agency's 19 hubs across the country.
PPE was also an initial challenge for Hallelujah General Hospital, the second to have received a license for COVID-19 treatment from the government. Hallelujah, which also provides services like dialysis treatments for kidney problems found only at a handful of institutions in the country, had started preparations for the pandemic much earlier as well.
Training and distribution of lifesaving PPE for its 40 medical staff were first on the to-do list. This was even prior to March 14, the date when the first positive COVID-19 case was recorded in the country, according to Kaleab Dereje (MD), assistant medical director at the Hospital.
It also donated its branch in Arat Kilo for government use along with equipment and health professionals, incurring a monthly cost of 1.2 million Br a month, according to him.
The prices here too, like any private hospital, are high, and options for a single bed, double bed and even the VIP treatment are on offer to patients. But for those who cannot afford it, the Hospital's COVID-19 treatment unit medical director states that referrals to the five public institutions have so far been smooth with no visible delays.
Even so, the laws are adapting to the quickly shifting landscape of COVID-19 healthcare. A new manual is operational as of last week, relaxing specifications for running a COVID-19 centre and lifting the price cap on items related to COVID-19 treatment.
The revision rescinds regulations like necessitating a separate building for COVID-19 treatment and instead targets integrated case management to allow both COVID-19 and other treatments to continue simultaneously. The risks are minimised as the manual dictates a higher patient to health professional ratio than before.
The rationale behind this is to meet the needs of non-COVID-19 patients. More importantly, it looks to encourage more private health providers to join and foster competition, which is hoped to regulate costs in a price cap.
The decision to reverse the older manual also comes bearing what the Ministry states is a better capacity for receiving patients. In December, ICU beds in public hospitals and health centres were filled to the brim with 13 people in line waiting for mechanical ventilators. Last week, there were idle ventilators across public hospitals in the country, according to data from the Ministry. With the chances of recovery for a person on mechanical ventilation at around five percent, this could be interpreted as either a good or a bad data point.
Hallelujah Hospital has so far successfully treated 300 people since commencing operations. Mechanical ventilators, needed for the most severe cases, are rare here much like anywhere else in the city, and the Hospital has been getting patients referred at very critical stages when chances of survival are low.
"It does give us confidence in our capabilities to care for patients on the one hand," said Natnael Fitsum (MD), Hallelujah's COVID-19 treatment unit medical director.
Even so, the private sector's involvement is lauded by many healthcare experts, especially seeing as the need for patient-centric care is on the rise.
The best way to ensure this need is met is to engage the private sector, according to Tegbar Yigzaw (MD), a public health specialist and president of the Ethiopian Medical Association.
"The supplementary support is good for the country, even in times of regular procedure, let alone emergencies," said Tegbar. "The private sector can also fill gaps in sub-speciality."
In the case of COVID-19, needs may not be adequately addressed through government efforts alone, according to the expert, who explained that there is definitely demand for private care among those who can afford it.
"The authorisation by the government, though arguably late, is the right decision," he said.
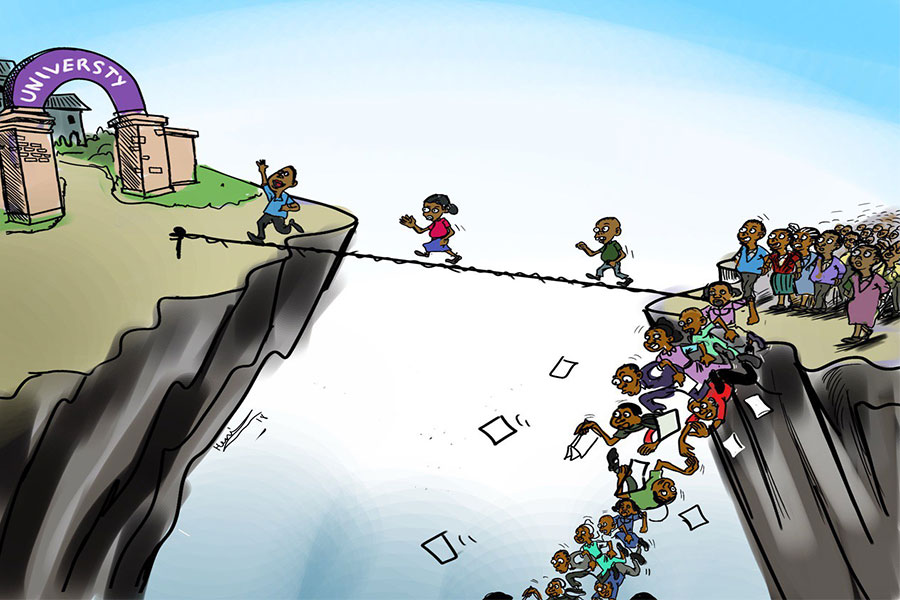
Tegbar maintains that quality care should come alongside affordability, adding that treatment costs should not leave patients bare-handed afterwards. The rising cost of healthcare is concerning, especially when less than one percent of the country's population can afford to access it, remarked Tegbar.
PUBLISHED ON
Jan 30,2021 [ VOL
21 , NO
1083]

Radar | Jan 04,2020

Editorial | Aug 30,2025

View From Arada | Dec 28,2019

Radar | Sep 10,2023

Verbatim | Jun 15,2024

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
Four years into an experiment with “shock therapy” in education, the national moo...