
My Opinion | Nov 23,2024
Jan 5 , 2019
By Belay Abera
It is not uncommon to hear of blunders within hospitals in Ethiopia. Admitted patients are sometimes misdiagnosed or given improper treatment. Sometimes medical mistakes could be committed as well.
References would be futile given that, from time to time, there is a significant enough medical mistake that it would take over the airwaves. People would be outraged, and officials would vow the institutions would be held accountable. But weeks, in some cases days, pass by and it would be forgotten, at least until the next major medical error.
Perhaps the more worrying problem is that of being misdiagnosed. This in some cases means being treated for a disease one does not have. In its non-fatal but painful way, most of us have had such experiences. But the more worrying problem is the issue of not being treated to begin with; of being told that we are fit when we are not.
Fortunately, this is not a problem only patients or the public is crying against. There are sinceres call from the medical community and the Ministry of Health to pay as much attention to quality as well as quantity and regulate private medical institutions more strictly.
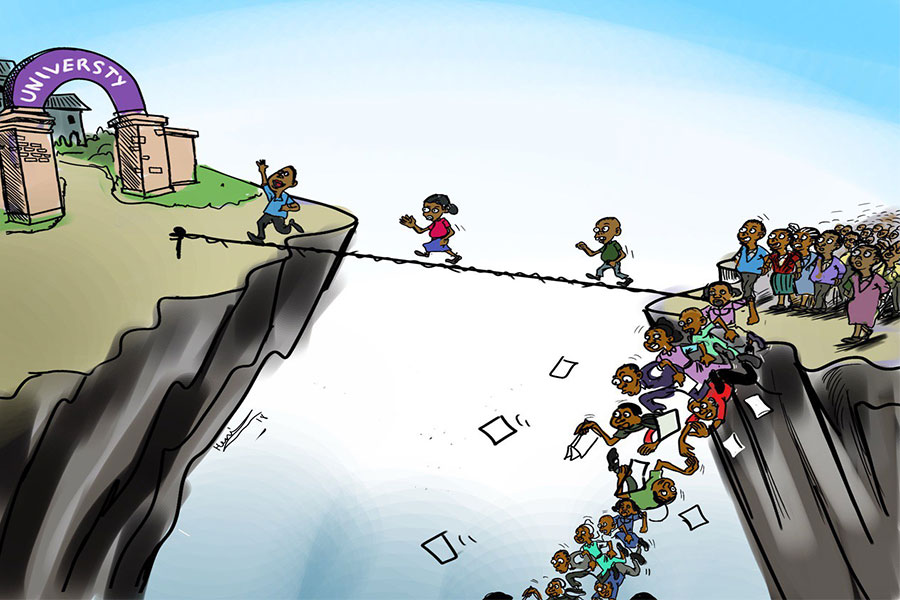
The tension is apparent when it comes to the industry. In a country where there are a million people for every 22 doctors, according to World Atlas, the chief priority of the government is perhaps to improve access to health coverage across the country as much as possible.
The investments in this regard are no doubt impressive. The nation currently has 3,400 health centres, an increase by over 600pc from a decade ago. Child and maternal mortality rates have declined, and there have been impressive achievements when it comes to containing HIV/AIDS, malaria and polio. This is not to mention the proliferation of specialist clinics, from eye to dermatology centres.
It is unfair to look at the problem merely from the perspective of the medical industry. It cannot be maintained that in a country with poor infrastructure and such low rates of medical practitioners, mistakes could be avoided if only the Health Ministry would do its job better. It is hard to sustain high standards of healthcare when there is no electricity to preserve vaccines or medicines or when a doctor has an overly crowded schedule.
Despite the mountainous challenges though, there is still room for improvement. Tinkering with hospital policies and instituting innovative ways of attending to problems can go a long way in securing quality in health care without compromising on quantity.
Lessons can be taken from the promising investment by the Health Ministry on drones for the supply of medical cargo to places that are far from town. It should serve as a valuable lesson on how with limited resources, efforts can be made to address challenges until a more sustainable solution can be arrived at, in this case, infrastructure that connects rural areas.
The means of improving quality has to start by coming up with ways of reducing misdiagnosing or mistakes.
Technology could be a very important tool here as well. Since misdiagnosing has to do mainly with how doctors perceive what the symptoms of their patients are, the Ministry could recommend that hospitals make use of diagnosing applications and software currently available in the global market.
They should also be encouraged to improve and digitise their data keeping capabilities, which could go a long way in understanding the history of patients’ health to make better diagnoses. Even better, information sharing among hospitals on a centralised server can produce better results. It can also show if whether or not new prescriptions will bode well with any possible allergies or a medicine currently being taken by the patient.
Communication failures cause some mistakes. These include errors in the reading of prescriptions by pharmacists. There are efforts underway to increase the use of computers in hospitals to avoid such mistakes and help patients get the correct medicine and at the correct dosage. This is a welcome respite from medical doctors’ famously bad handwriting.
PUBLISHED ON
Jan 05,2019 [ VOL
19 , NO
975]


My Opinion | Nov 23,2024

Fortune News | Dec 19,2018

Radar | May 16,2020

Radar | Mar 02,2019

Radar | Sep 10,2021

Radar | Aug 29,2020

Agenda | May 11,2019

Fortune News | Sep 21,2025

Radar | Feb 18,2023

Viewpoints | Apr 17,2021

Photo Gallery | 175319 Views | May 06,2019

Photo Gallery | 165543 Views | Apr 26,2019

Photo Gallery | 155868 Views | Oct 06,2021

My Opinion | 136804 Views | Aug 14,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
Four years into an experiment with “shock therapy” in education, the national moo...
Oct 18 , 2025 . By NAHOM AYELE
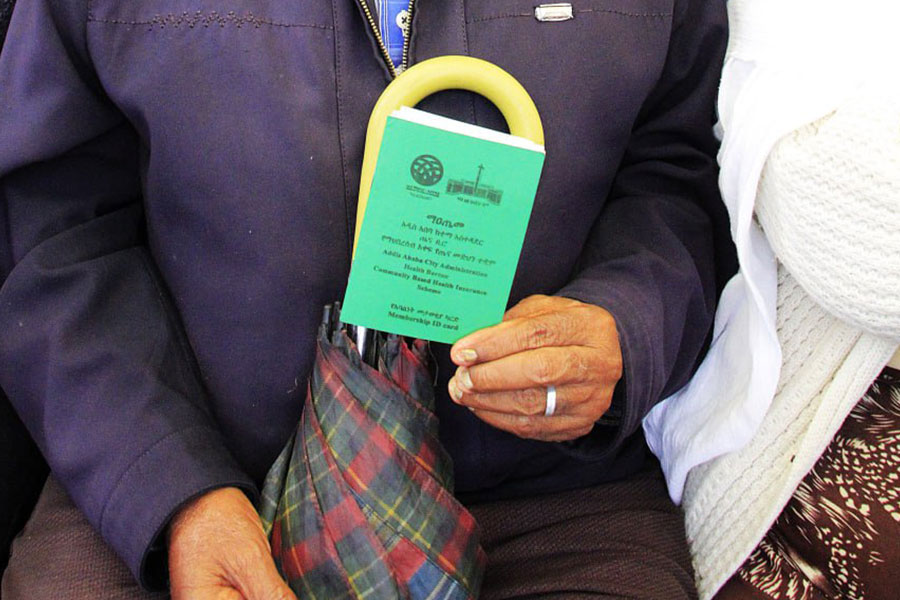
In a sweeping reform that upends nearly a decade of uniform health insurance contribu...

Oct 18 , 2025 . By BEZAWIT HULUAGER
A bill that could transform the nutritional state sits in a limbo, even as the countr...

Oct 18 , 2025 . By SURAFEL MULUGETA
A long-planned directive to curb carbon emissions from fossil-fuel-powered vehicles h...

Oct 18 , 2025 . By BEZAWIT HULUAGER
Transaction advisors working with companies that hold over a quarter of a billion Bir...