
Commentaries | Aug 05,2023
Feb 10 , 2024
By Ellen Johnson Sirleaf , Jean Kaseya
As African leaders convene in Addis Abeba, the pledge to deploy two million community health workers (CHWs) comes into sharp focus. With Africa projected to face a six million health worker shortfall by 2030, the continent's health infrastructure is on the balance, warn Ellen Johnson Sirleaf, a former president of Liberia, and Jean Kaseya, director-general of the Africa Centers for Disease Control & Prevention, in this commentary provided by Project Syndicate (PS).
The pledge made by Africa's leaders in 2017 to deploy two million community health workers (CHWs) marked a significant recognition of the essential role these workers play in advancing health across the continent. Seven years into this commitment, as leaders prepare to gather in Addis Abeba, a critical evaluation of progress is necessary. With a projected shortfall of six million health workers by 2030, the importance of CHWs in bridging Africa's health service gaps cannot be overstated.
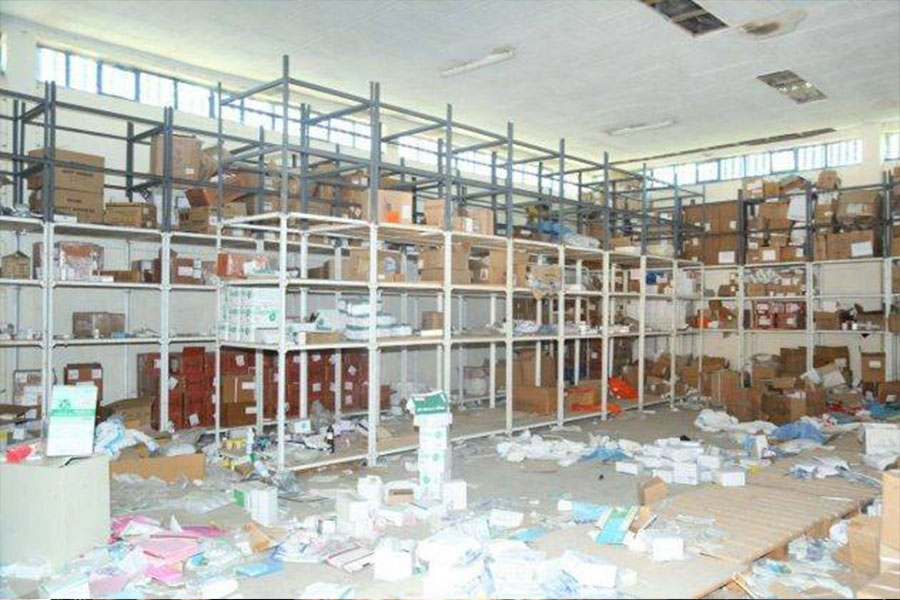
The urgency to develop resilient community health-worker programs across the continent has escalated in the face of this looming crisis. We have witnessed how disease outbreaks can plunge a country into darkness – and how the power of CHWs can help pull it back into the light. Liberia's experience shows that community health workers need adequate resources and financial support to be effective. In the early 2010s, Liberia's efforts to offer primary health care in remote areas faced significant challenges. There was a shortage of health workers, and where CHWs were deployed, they were under-compensated. They did not have the necessary equipment or training to deliver the essential care that was so desperately needed.
As a result, different community health initiatives run in parallel by the government and other stakeholders failed to significantly impact patients – a common problem in many African countries.
In 2016, the Liberian government launched the National Community Health Assistant Program to address these issues and apply the lessons learned from the Ebola outbreak that began in 2014. With proper supervision, adequate salaries, and enough supplies to reach every household in their communities, community health workers were empowered to provide standardised, integrated primary healthcare services. The results speak for themselves.
Liberia's 4,000 community health workers now deliver nearly 50pc of all reported malaria treatments for children under five and consistently provide access to health services, even during the COVID-19 pandemic. Programs that take a similar approach have yielded positive results in other African countries.
Since Ethiopia implemented its community-based Health Extension Program, which has deployed 40,000 community health workers, vaccination rates have tripled, and child mortality has fallen dramatically. The experience of these and other countries shows that supporting health workers and integrating them into national health systems can save lives and create livelihoods. It should serve as a guide for expanding community health services across the continent.
A resilient community health workforce is key to overcoming existing and future health challenges in Africa, which currently range from alarming maternal and infant mortality rates to a high burden of communicable diseases. Equally worrying is the escalating climate crisis, which has underscored the urgency of improving access to care and building health systems adapting to a changing environment. Increasing the number of community health workers, and ensuring that they have adequate resources, is one of the most cost-effective and sustainable ways to achieve these goals.
Unfortunately, a daunting 4.4 billion dollar annual funding gap – compounded by fragmented financial flows – continues to slow our progress toward a healthier, safer, and more prosperous Africa. The solution is to adopt a "one plan, one budget, one report" framework, like that used by Liberia and Ethiopia. With this approach, governments outline their strategies for national community health programs, and partners coordinate resources and technical expertise to reduce the bureaucratic burden.
The Africa Centers for Disease Control & Prevention (ACDCP) and partners launched the first-ever continental coordination mechanism for community health in November 2023. Encouraging coordination among stakeholders will enable African countries to build effective and efficient community health worker programs to tackle the challenges of high-burden communicable diseases such as HIV, tuberculosis, malaria, and non-communicable diseases, as well as to respond better to emergencies, including epidemics and climate shocks.
The Africa CDC remains firmly committed to strengthening the community health workforce, which dovetails with the New Public Health Order – the organisation's health-security agenda – and the Afric Union's (AU) initiative to deploy two million additional community health workers on the continent. As part of this effort, the Africa CDC has collaborated with Africa Frontline First to mobilise the financing needed to professionalise community health workers.
Last year's Reaching the Last Mile Forum in Dubai was a success on that front: 12 partners committed to accelerating support for professional community health workers. The announcement also included 900 million dollars from the Global Fund over the next three years, 74pc of which is earmarked for Africa.
The private and public actors in Africa must take coordinated action. As heads of state convene for the AU Summit, we urge them to make developing an integrated professional community health workforce a top priority, with clear success metrics to enable data and evidence to be shared with member states. This will promote a culture of continuous learning and standardisation of CHW programs across Africa.
Community health is the key to a more prosperous, healthier Africa. We must seize the opportunity to train and deploy a robust corps of community health workers.
PUBLISHED ON
Feb 10,2024 [ VOL
24 , NO
1241]

Commentaries | Aug 05,2023

Radar | Apr 27,2025

Fortune News | Jul 26,2025
Fortune News | Aug 25,2024

Viewpoints | Jun 10,2023
Fortune News | Dec 19,2021

Viewpoints | Sep 23,2023

Fortune News | Nov 21,2020

My Opinion | May 08,2021

Radar | Sep 19,2020

Photo Gallery | 179922 Views | May 06,2019

Photo Gallery | 170119 Views | Apr 26,2019

Photo Gallery | 161108 Views | Oct 06,2021

My Opinion | 137231 Views | Aug 14,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Nov 1 , 2025
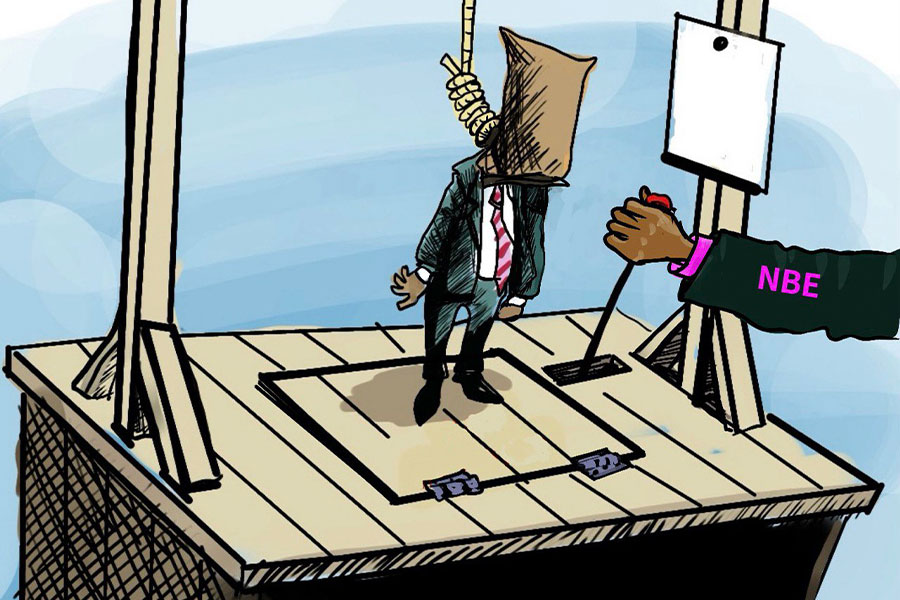
The National Bank of Ethiopia (NBE) issued a statement two weeks ago that appeared to...
Oct 25 , 2025
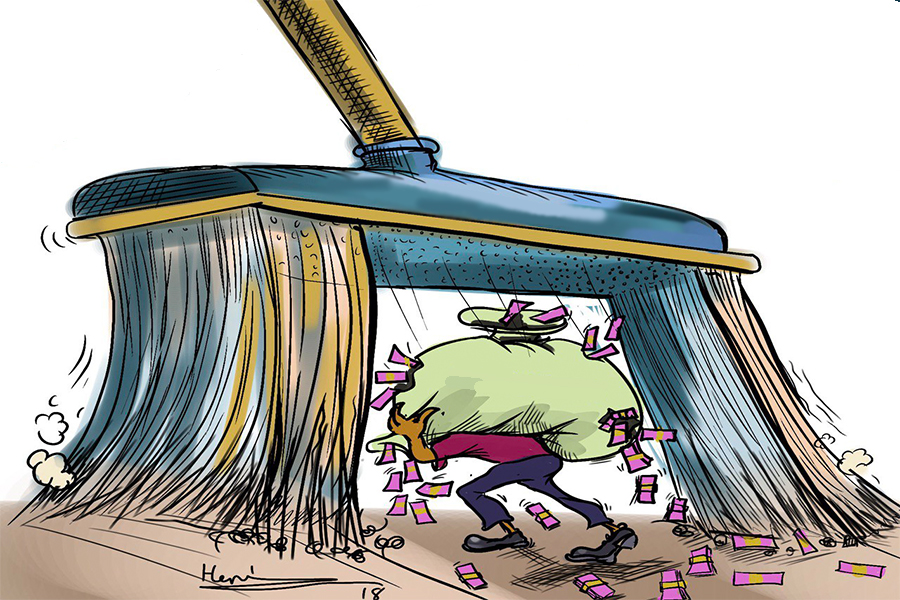
The regulatory machinery is on overdrive. In only two years, no fewer than 35 new pro...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Nov 2 , 2025
The National Bank of Ethiopia (NBE) has scrapped the credit-growth ceiling that had s...

Nov 2 , 2025 . By SURAFEL MULUGETA
The burgeoning data mining industry is struggling with mounting concerns following th...

Nov 2 , 2025 . By YITBAREK GETACHEW
Berhan Bank has chosen a different route in its pursuit of a new headquarters, opting for a transitional building instea...

Nov 2 , 2025 . By BEZAWIT HULUAGER
Nib International Bank S.C. has found itself at the epicentre of a severe governance...