Jun 1 , 2019
By Abiy Seifu Estifanos
Ethiopia’s health sector has made remarkable progress in the span of 10 to 15 years. It has managed to increase the number of health posts to more than 16,000, health centres to more than 3,500 and hospitals to close to 400 from a very low baseline.
Thousands of health workers (medical doctors, health officers, pharmacists, midwives, clinical nurses, health extension workers, etc.) have been trained and deployed. A good chunk of money was mobilised from the global community, national treasure and out-of-pocket and pumped into the health system.
As a result, although uneven across regions, huge gains were made. The potential health coverage was increased. The suffering of millions was prevented, and the lives of mothers, children and adults were saved. All these should be celebrated and the Ministry of Health and its subsidiaries should be given credit for leading the system!
And, yes, this has been talked about by many of us in the system and oftentimes exaggerated to cover up the gaps. Writing an expanded note on this good news is parroting the boring narrative of the last couple of years. I would rather talk about the problems and challenges, and what we can do about them.
I am an optimist. I like to see the glass as half-full. But that doesn’t mean the glass should remain unfilled. It is time to break the bad news, as a problem that is not acknowledged cannot be fixed.
Reviewing the various national and sub-national surveys, studies and assessments, one would feel enormously depressed. The health system is poorly managed, the meager resources of the country are wasted, and mediocrity is engulfing the once revered health profession. Problems in our health system are systemic, leaving none of the six WHO health system building blocks unaffected.
Take the case of services: this component is about making affordable quality health services available to society. For the rural society, the voiceless majority, with the modest expectation of quality health service, seeking care from health facilities continues to be the last resort. They come to us after trying out all possible traditional options at home or in the community.
It is unfortunate that health facilities are not yet their primary preference. When they rarely come to health facilities, they are not provided with affordable quality health services. They are not treated with the dignity and respect they deserve. Let’s be frank! The smiling and compassionate faces of health professionals plastered on TV ads, posters and at the leadership retreat parties are nowhere to be found in the wards and clinics. As a result, health service utilisation remains poor.
Particularly, health centres are hugely underutilised. The few people who visit the health facilities for clinical care prefer hospitals – overburdening them. Some "joke" that the health centres became "Kana centres".
I think it is obvious that the Health Extension Program (HEP) has long hibernated, who knows when it will wake up. HEP palpates with vibrancy only in the minds of its creators or those who make their living by portraying a rosy picture of the program. It seems it is on its deathbed, silently dying.
Thinking about the Ethiopian health workforce leaves you with mixed feelings. While celebrating the successes in manning the sector with so many personnel so quickly, the system has also set itself up with great challenges. Some of these will be around for a long time to come. Some are irreversible.
We now know that the lame argument that "we should first reach high coverage and worry about quality later" was absolutely wrong – it is a miserably failed model. It instead created a perfect culture to breed mediocrity. As a result, we see now a lot of people in white gowns who are unable and/or unwilling to provide care. All of us are to blame for allowing this to happen.
Due to the sub-standard training, the majority of the poorly trained health workers have sub-standard competence and parochial conceptualization of the health system and the society in general. The training failed to capacitate them to be resourceful to solve problems with local solutions. Externalisation and inaction became their second nature.
Besides, we are given limited opportunities for mentoring and transferring skills from senior health professionals to juniors. Tensions and conflicts were allowed to brew among different health professionals partly due to confused and overlapping roles given to them.
While it is well known that health care cannot be successful without excellent team spirit and teamwork, they were forced to compete for limited opportunities rather than cooperate to create ample opportunities for everyone.
Health Management Information System (HMIS) is the sensory organ of the health system. We hear, see, touch, smell and taste the fruits of our investment through the HMIS. Unfortunately, our culture and attitude toward accurate recording and reporting of what we do have descended from bad to worse.
As Ronald Coase said, “If you torture the data long enough, it will confess to anything." Politicians were allowed to torture the data, so it confesses to their illusion. They were allowed to fabricate data to the extent that lying has become the norm. It is now a systemic disease.
To cure the data disease, the politicians leading the health system have to first acknowledge the cost of lying – the harm lying brings to the health system, the country and society.
If not cured soon and intensively, false reporting will perpetuate itself. It will metastasize to academia and civil societies. With mediocrity propagating to academia and civil society, this is not a distant future risk. It is around the corner.
Without accurate data, we are lost in the dark. The second-rate cadres and corruptors will take over the system. The system will eventually collapse. We have to protect the health system data, by any means. Demolish the data torture houses and free the data.
There is a long list of essential drugs and supplies. As the language and discourse changes from ‘coverage’ to ‘quality’, the list continues to expand. Compared to what was there a couple of years ago, a lot has been invested to make essential drugs and supplies available. We are by far in a better position now than ever.
However, the stockout of essential drugs and supplies is not a rare phenomenon. When big brother forgets to buy or ship them on time you may not even find some of the drugs and supplies in the whole country, even when you have the money to buy them. Quantification, procurement, and supply chain management are weak.
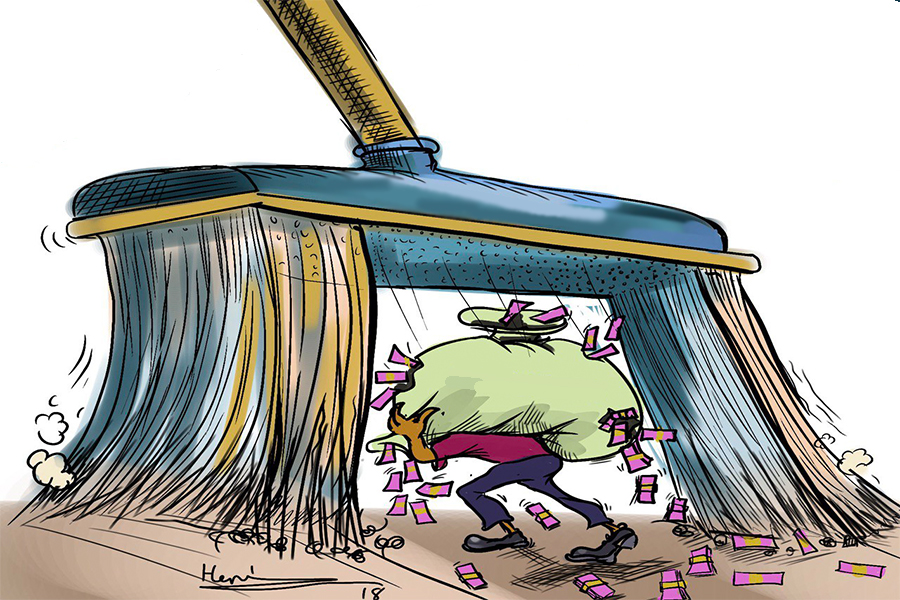
Besides, there is a lot of wastage. The weak system coupled with a lack of accountability invited corruptors to the system with open arms and allowed them to exploit the sector. Corruptors do not have a heart for dying patients. They only care about the money they make.
In the last 29 years, the population of Ethiopia has more than doubled (from 48 to 108 million) and so has the potential demand for health care. The money that was invested in the system might have increased at a higher rate compared to other social sectors but, for sure, falls far short of meeting the increasing demand.
Although the government’s contribution to health care financing has nominally increased, the health system continues to depend on out-of-pocket payment from users and money from health development partners. Contributory financing – the social and community-based health insurances and user fees schemes – are struggling to stand on their feet in the face of weak capacity of the Ministry of Health and its local subsidiaries.
In the era of Trump and Brexit, planning your health care on external assistance is not only unwise but also risky. The health system needs an innovative financing strategy that should quickly transition its dependence to mainly domestic resources.
Leadership and governance is a neglected component of our health system. With just good leadership and governance a lot can be gained, even in resource limited settings. The disease that made the above five health system components sick can be cured (or at least its effects largely reduced) by improving the leadership and governance of the health system.
A system is made of people. To make it effective, people need to subscribe to a common vision of the health system and roll up their sleeves to work. For this to happen, a leader needs to be trusted – both for his capacity and intention. In a system where nepotism, political affiliations and other criteria rather than merit are used to assign people in leadership positions it will be next to impossible to build trust.
The health system’s leadership and governance have rotted and crumbled. In order to change this and reinvigorate the health system, nepotism and politics need to be kicked out of it. It has to be kept professional.
It can be argued that it is impossible to completely remove politics from the health system because, after all, it is political parties that form the government. That is true. But we can keep it to the minimum possible level and eliminate its negative effect on health care, particularly in health facilities where patients receive care. You cure diseases by providing evidence-based, high-quality healthcare. You can't kill bacteria and viruses by murmuring your confused political ideologies.
To remedy all these health system maladies, something serious has to be done. Martin Luther King, Jr. is quoted as saying “History will have to record that the greatest tragedy of this period of social transition was not the strident clamour of bad people but the appalling silence of good people”. I wrote the above not because I am an expert on the health system, but because the health system's scientists, if there are any, preferred to keep quiet.
PUBLISHED ON
Jun 01,2019 [ VOL
20 , NO
996]


Commentaries | Jul 18,2021

Fortune News | Mar 13,2021
Agenda | Feb 04,2023

Fortune News | Dec 25,2021
Sunday with Eden | Oct 19,2019

Sunday with Eden | May 13,2023

Radar | Nov 02,2025

Commentaries | Feb 29,2020

View From Arada | Jan 24,2021

Fortune News | Jun 19,2021

Photo Gallery | 180459 Views | May 06,2019

Photo Gallery | 170658 Views | Apr 26,2019

Photo Gallery | 161715 Views | Oct 06,2021

My Opinion | 137285 Views | Aug 14,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Nov 1 , 2025
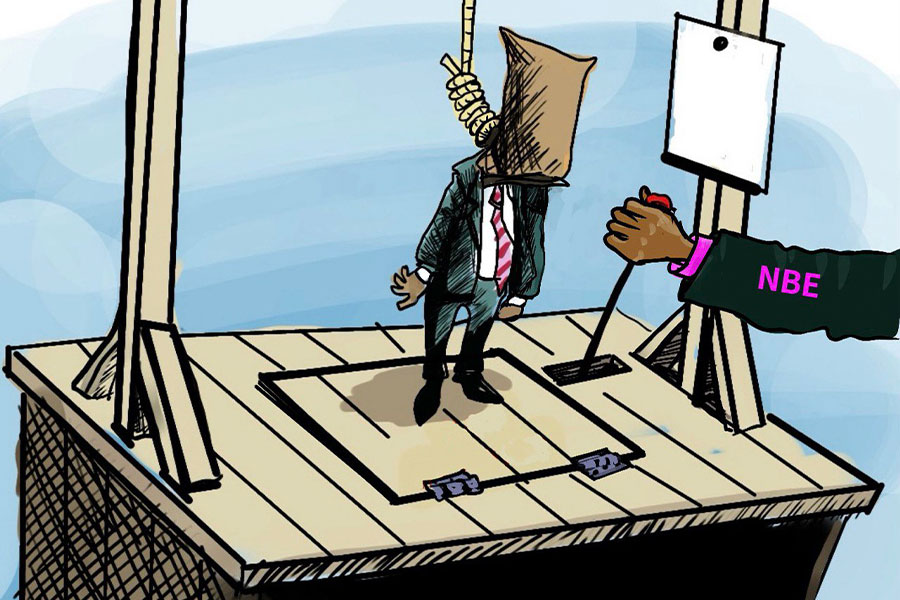
The National Bank of Ethiopia (NBE) issued a statement two weeks ago that appeared to...
Oct 25 , 2025
The regulatory machinery is on overdrive. In only two years, no fewer than 35 new pro...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Nov 2 , 2025
The National Bank of Ethiopia (NBE) has scrapped the credit-growth ceiling that had s...

Nov 2 , 2025 . By SURAFEL MULUGETA
The burgeoning data mining industry is struggling with mounting concerns following th...

Nov 2 , 2025 . By YITBAREK GETACHEW
Berhan Bank has chosen a different route in its pursuit of a new headquarters, opting for a transitional building instea...

Nov 2 , 2025 . By BEZAWIT HULUAGER
Nib International Bank S.C. has found itself at the epicentre of a severe governance...