
Photo Gallery | 180345 Views | May 06,2019
May 24 , 2025.
Public hospitals have fallen eerily quiet lately. Corridors once crowded with patients' relatives now echo, wards lie half-empty, and family members milled outside in anxious knots. The silence was not the result of medical efficiency but of absence. Medical professionals, mainly doctors, have downed tools.
Their nationwide strike, launched after years of pleading for “better wage structure and incentive systems”, has already run for over a week, leaving desperate patients to fend for themselves.
No one could doubt why the walk-out happened. “Livable wage” has become the rallying cry of professionals who feel condemned to financial indignity.
A public hospital in Addis Abeba advertised 50 posts for freshly minted general practitioners last week, offering a gross monthly salary of 10,600 Br, about 80 dollars at last week’s exchange rate. That sum scarcely covers a month’s rent for a cramped public condominium, let alone food or transport. Nurses fare worse, pocketing as little as 4,000 Br and 6,000 Br. By contrast, a doctor in private practice can earn up to 25,000 Br.
Leaders of medical associations set matters in train in the second week of April this year, lodging a 12-point petition with the Ministry of Health (MoH), under Mekdes Daba (MD), and threatening a nationwide strike if no answer came within a month. Among their grievances are crumbling equipment, chronic shortages of supplies and the grim reality that, in remote facilities, staff are compelled to improvise basic tools.
The ultimatum expired two weeks ago. Silence met it. Officials replied only that abandoning a life-saving vocation was “unethical” and “illegal”, urging sacrifice today for the “prosperity” of tomorrow.
When white coats finally walked out, the authorities reached for coercion. Police detained prominent physicians, close to 47, and courts swiftly arraigned them. Administrative orders demanded that staff report for duty or face dismissal. Fresh graduates were hustled in to plug the gaps, a stop-gap that may keep lights on but hardly compensates for seasoned expertise. Such tactics, tried and failed by governments everywhere, can only deepen mistrust and do nothing to treat the underlying malaise.
That malaise extends far beyond wages.
The federal health budget looks impressive at first glance, rocketing from 2.4 billion Br in 2006/07 to 100.2 billion Br this fiscal year and rising by almost 26pc in nominal terms in 2023/24 alone. Yet, inflation running close to 20pc (YoY) has eroded purchasing power. Adjusted for prices, last year’s budget allocation actually shrank by roughly three percent. Spiralling costs have eaten into every line-item, none more so than wages.
Meanwhile, the country boasts more than 400 hospitals, 3,900 health centres and over 15,000 health posts. In the 13 years beginning in 2010, the number of hospitals doubled, and health centres expanded by more than 30pc. The healthcare workforce has swollen, too, from about 4,000 doctors a decade ago to nearly 20,000. But the population has grown even faster, exceeding 100 million. One doctor is for every 5,843 citizens, far below the World Health Organisation’s (WHO) minimum of one per 1,000. The ratio of nurses and midwives, at about one per 1,000 Ethiopians, is scarcely better.
Shortages bite hardest on the periphery. In Somali and Afar regional states, scarcely any newcomer is willing to accept a posting. Modest housing allowances and tiny rural top-ups have failed to lure recruits. Even flagship urban hospitals struggle. At Tikur Anbessa Specialised Hospital, nurses in the maternity ward routinely juggle twice the recommended patient load. Some take home only 5,000 Br a month, barely enough for rent and basic food.
Physical structures may multiply, but without motivated staff, they are hollow shells.
External money props up much of the system, with donors covering 34pc of total health spending in 2020, for instance. However, geopolitical ructions and tighter budgets abroad are already squeezing that lifeline. Community-based health insurance (CBHI) now covers over 11 million households and was meant to shield citizens from ruinous bills. However, out-of-pocket payments still make up roughly one-third of overall expenditure.
Insurance cards would become worthless paper if doctors and nurses deserted public facilities.
Understandably, federal officials plead fiscal constraint. Ethiopia devotes a mere 36.4 dollars for a person to health each year, among the lowest in sub-Saharan Africa and far short of the regional average of 98 dollars. Inflation has blown a hole in pay packets across the public sector, and the federal government is wrestling with debt, war’s aftershocks and the costs of economic liberalisation. After all, it sits on a budget deficit for the 2024/25 fiscal year of 2.1pc of GDP, with total deficit financing requirements reaching 281 billion Br. This was even before Parliament approved an additional spending totalling 581.98 billion Br.
Nonetheless, refusing to confront the wage crisis rocking the medical community risks undoing decades of gains in vaccination, maternal health and disease control.
Better pay should be seen as no mere matter of fairness. For thousands of doctors and nurses, it is an existential issue. A stable and adequately rewarded workforce would cut turnover, curb brain drain, and improve outcomes, as well as investments that yield returns in productivity and growth. Even modest concessions could soothe tempers. The authorities might permit limited private practice for public-sector clinicians, expand performance-based bonuses or cultivate public-private partnerships to share revenues more equitably.
However, money alone will not fix everything in the long run. The strike is only the latest manifestation of broader political and economic governance problems. The administration funnelled scarce resources into showcase projects while neglecting investments that boost national productivity. Inflation, fuelled partly by rapid economic policy liberalisation and weak supply responses, has savaged household budgets. When bread and rent gobble a salary, appeals to patriotic sacrifice can only ring hollow.
At our press time late last week, the stand-off continued, with courtrooms processing detained medics, and ministers scrambling to keep facilities open. Each day of paralysis erodes public trust and imperils lives. These are days when babies are delivered without skilled attendants, chronic patients are skipping dialysis, and emergencies are turning fatal for want of a surgeon. The human cost of underpaying health professionals should be measured beyond the Birr saved but in lives lost.
Unless the authorities and striking medical workers find common ground soon, the exodus of talent will accelerate. Thousands of Ethiopians already sit examinations for posts in the Gulf, Europe and beyond, lured by wages that can be 10 times higher. Every departure represents years of subsidised training gone to waste and another widening gap on the ward.
Negotiation remains the obvious first step. The medical associations have shown they can organise and compromise if met in good faith. A phased wage rise tied to clear targets and financed through reallocation within the existing budget could be a helpful start. So would transparent timelines for upgrading equipment and restoring supply chains.
In the longer term, Prime Minister Abiy Ahmed's (PhD) administration needs to rethink its economic policy priorities. Health spending cannot be considered a luxury to be postponed until growth is attained. It is a foundation for growth itself. So is respect for professional dignity. A government that quells dissent with batons and court summonses may win a day, but it will lose the commitment of the very people on whom public welfare depends.
The struggle unfolding in hospital corridors should be viewed as more than pay slips. It is a test of whether the administration can match lofty promises of prosperity with the practical needs of its citizens. If doctors and nurses cannot feed their own lot, they will leave, or stay home. Either way, patients will pay. The country’s impressive skylines and manicured asphalt roads will stand as monuments to misplaced priorities.
Ethiopia has made great progress in expanding access to healthcare over the decades. Letting that progress unravel for lack of a credible wage policy would be a tragic false economy. If it continues, the silence in the wards will echo loudest not in empty budgets but in the grief of families left untreated.
PUBLISHED ON
May 24,2025 [ VOL
26 , NO
1308]

Photo Gallery | 180345 Views | May 06,2019

Photo Gallery | 170543 Views | Apr 26,2019

Photo Gallery | 161578 Views | Oct 06,2021

My Opinion | 137274 Views | Aug 14,2021
Nov 1 , 2025
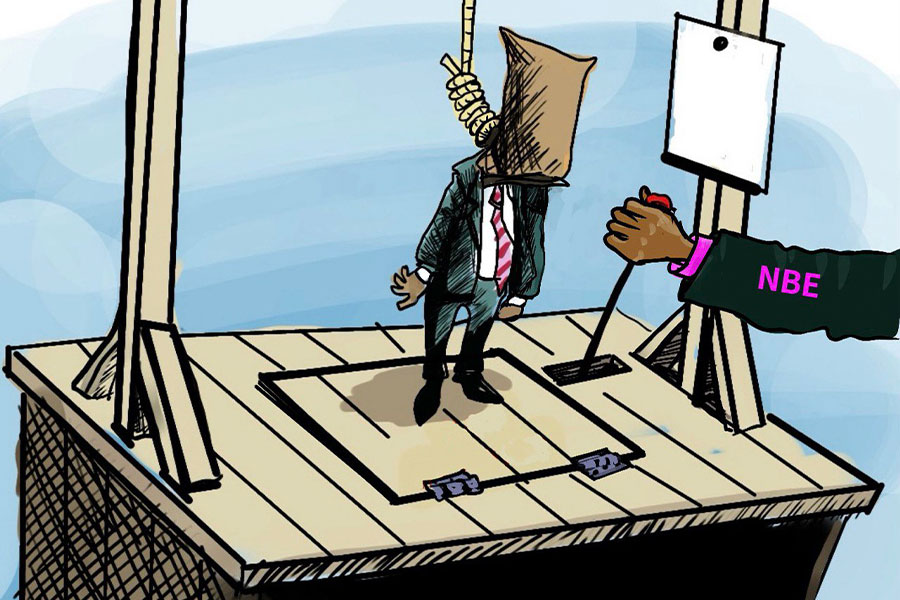
The National Bank of Ethiopia (NBE) issued a statement two weeks ago that appeared to...
Oct 25 , 2025
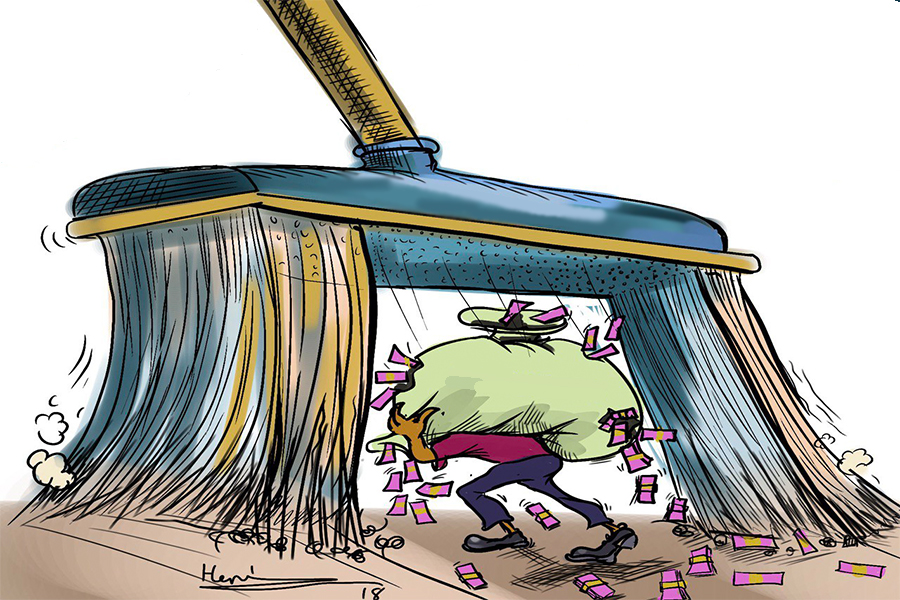
The regulatory machinery is on overdrive. In only two years, no fewer than 35 new pro...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...