
Advertorials | May 30,2025
An attendant at Minelik II Referral Hospital, Kindu Berihun was shocked by the cost of surgery needed for his relative. The patient, a 28-year-old bartender was rushed to the hospital last week due to severe abdominal pain and was scheduled for surgery the same day.
He recently moved to Addis Abeba from Gonder town, Amhara Regional State. Kindu and other family members chose the public hospital, assuming it would be less expensive than private options.
"It makes no difference," Kindu said.
He was dismayed about having to source surgical materials, including gloves, syringes, and critical supplies like normal saline, from outside the hospital as in-house pharmacies were out of stock.
"It was more than we could handle," he told Fortune. "But we managed to borrow from friends."
Though hopeful for a successful surgery, the financial burden weighs heavily on Kindu, who is concerned about how to cover future medical expenses if ongoing care is required.
The issue is not limited to Minelik Hospital. Medicine shortages have been an issue for public hospitals and pharmacies. According to officials, the problem stems from a mismatch between budget allocations and service delivery needs, compounded by inflationary pressures and supply chain disruptions.
Tikur Anbessa Specialised Hospital (TASH), the country's largest referral hospital, wrestles with a limited budget despite handling over 15,000 patients. Demisew Gezahegn, the pharmacy director, described the medicine supply concern as complex and strained. He noted shortages of essential medications, including some cardiac, psychotic, and antibiotic drugs, due to budget constraints.
"We don't have Ringer's lactate right now," he said.
While noting that normal saline can be used as a substitute for Ringer's lactate, notable differences hinder proper procedures.
According to Demisew, they have not received medicines since July. He underscored that the Hospital’s budget for medication is only 60 million Br—about one tenth of the amount needed. He believes the delay between applying for additional funds and the actual procurement of medicines exacerbates the issue.
TASH also relies on donations for chemotherapy medications, which are too expensive to be covered by the Hospital’s budget. Nilotinib, used to treat a type of blood cancer, is currently required for 120 patients with leukaemia at the Hospital. Even with a government subsidy covering half the cost, 29 million Br is needed annually for these patients—amounting to half of the Hospital's annual budget for medicines.
Andualem Deneke (MD), chief executive director of Tikur Anbesa Health Science College, ascribed that the hospital procures medicines and medical equipment primarily through the Ethiopian Pharmaceuticals Supply Service (EPSS), but also relies on private companies, donations, and direct patient purchases when necessary. He suggests patients seek medicines from other sources.
"Developing countries like ours can't cover 100pc of medicine and medical equipment," he told Fortune.
Yekatit 12 Hospital is also facing shortages of fluids. The shortage has forced practitioners to improvise by mixing solutions, while those who can afford it purchase fluids outside the hospital. A social wing in the hospital also assists patients based on social worker assessments.
Adugna Mulu, pharmacy service director, confirmed a shortage of dextrose normal saline and Ringer's lactate, attributing the issue to supply chain disruptions at EPSS. When medicines are out of stock, Adugna said hospitals must turn to private traders, but price fluctuations and foreign exchange shortages complicate these efforts.
"Budget constraints are a major factor," Adugna said.
A total of 20 health institutions have an outstanding debt of 1.8 billion Br with EPSS, including St. Paul Hospital Millennium Medical College and Alert Hospital.
Ethiopian Pharmaceuticals Supply Service is the main supplier of medicines and medical equipment to over 5,000 healthcare providers, mostly public institutions. Awol Hassen, public relations officer, argues the shortage is not of supplies, attributing the problem to overlapping credits at hospitals. He disclosed that Tikur Anbesa alone has a credit of 110 million Br accrued until July, clarifying that EPSS withholds supplies when hospitals have unpaid debts.
"We make exceptions for emergencies," he told Fortune.
More than 12 local manufacturers supply 36pc of EPSS’s medicinal requirements, valued at over five billion Birr, with the remainder sourced internationally. EPSS plans to increase local manufacturing to 60pc. However, it faces supply challenges, including import delays and inaccurate forecasting, while spending one billion dollars annually on medicines and medical devices.
Research indicates that about 80 to 85pc of pharmaceuticals are imported. EPSS offers local manufacturers a price preference of up to 25pc, but local firms often fail to deliver the contracted amounts, fulfilling only 23.8pc of commitments. Local manufacturers face low production capacity and supply chain issues for input materials, underutilising their capacity and producing limited generic medicines without adequate research and development investment.
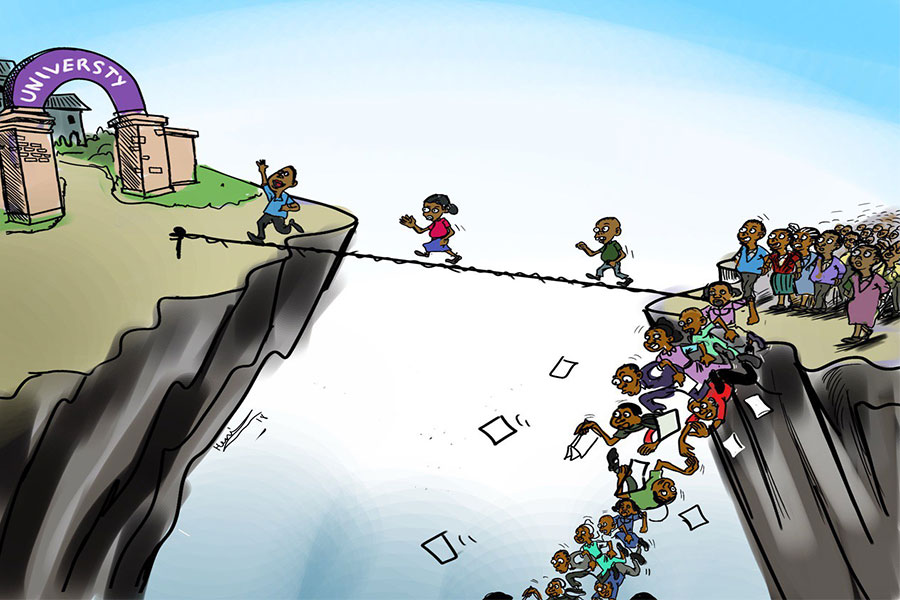
Although the World Health Organisation (WHO) recommends a minimum of 80 dollars a person annually for health expenditure in sub-Saharan Africa, Ethiopia's allocation is less than 40 dollars a person. The government, with support from international partners like USAID, is working to address these issues through reforms aimed at improving health financing, increasing subsidies, and piloting larger risk pools to create more sustainable insurance mechanisms. But, the road to achieving universal health coverage remains fraught with obstacles, particularly in ensuring equitable access to quality care and financial protection for all citizens.
Regassa Bayissa, a leading executive in medicine and medical devices at the Ministry of Health, pointed out that hospitals operate a revolving drug fund, allowing them to purchase and sell medications with a 25pc profit margin. However, Regassa said these funds are usually redirected for other uses.
He underscored that the Ministry has supported hospitals during pandemics and emergencies by distributing donated medicines and medical devices, which are supplementary to hospitals' main budgets. While pointing out that WHO recommends that a hospital’s medicine purchases make up 40pc of its total annual budget, Regassa said in Ethiopia, this typically ranges from five to 10pc.
To alleviate the financial burden for patients employed in the informal sector, Community-Based Health Insurance (CBHI) schemes were introduced in Ethiopia in 2011. The scheme has expanded, covering over 720 districts and nearly 41.6 million household members.
According to an article written by Esubalew Demissie, Laurel Hatt, and Ezinne Ezekwem in 2023, CBHI members gain access to a full range of healthcare services by paying an annual premium of 500 Br, reducing their out-of-pocket expenses. However, the authors argue the success of CBHI schemes has been uneven, with many facing financial difficulties due to limited enrollment rates and insufficient government subsidies. They indicate the schemes operate independently at the district level, resulting in fragmented risk pools that cannot support each other in times of financial strain, leading to some becoming insolvent.
This situation is further exacerbated by the poor quality of care in public health facilities, including frequent shortages of medicines and supplies, which deter potential members from enrolling in the CBHI. According to the article, many facilities struggle with unreliable infrastructure, a shortage of trained staff, and a lack of essential medical supplies and diagnostic services.
Getasew Amare, a health economist, underlined the weakened financial power of health institutions due to low budget allocations. He said public health institutions cannot freely adjust service fees, which are regulated by regional authorities.
"It is crippling the facilities," he said.
According to Getasew, the reimbursement fee is late or diminished for regional hospitals. He recommends hospitals explore ways to increase their income, such as strengthening private wing services and soliciting more donations. He said hospitals’ management needs to prioritise medicine and medical devices rather than paying allowances and spending money on reconstruction.
"It's about priority," said Getasew.
He suggested that granting hospitals autonomy from government regulation could help them adjust outdated pricing structures to better align costs with income, motivating improvements in service quality. The College of Health Science under Addis Abeba University begins its quest for autonomy riding on a bill under the formation of the University.
"It should be strictly regulated to fit the community," Getasew told Fortune.
PUBLISHED ON
Sep 01,2024 [ VOL
25 , NO
1270]

Advertorials | May 30,2025

Radar | Aug 03,2025

Agenda | Sep 10,2022

Agenda | Jul 17,2022

Commentaries | Jan 16,2021

Radar | Aug 13,2022

Fortune News | Jun 29,2025

Radar | Oct 31,2022

Fortune News | Aug 09,2025

Radar | Sep 14,2024

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
Four years into an experiment with “shock therapy” in education, the national moo...