
View From Arada | Jun 21,2025
Malaria is no stranger to Ethiopia. Every year, the disease poses a public health issue, especially in rural regions where the majority of the population lives in areas conducive to mosquito breeding. However, as the country wrestles with a sharp uptick in cases and fatalities in 2024, the ongoing crisis reveals deeper, systemic issues ranging from climate change and health infrastructure shortcomings to global supply chain disruptions.
Mandela Abiyu, a 24-year-old student from Butajira, Central Ethiopia Regional State, never imagined that a brief academic journey to Jinka General Hospital would bring him face-to-face with a disease that afflicts millions. He always considered himself to be “healthy as a horse,” recalling the years he lived without illness. But within days of arriving in the town, Mandela found himself bedridden, struggling with fever, loss of appetite, and severe weakness. He was diagnosed with malaria.
His case was complicated. Initially, only the weak species was detected, leading to treatment with a drug called chloroquine. With his symptoms like headache and appetite loss lingering, he was readmitted to the hospital for further testing. He said that doctors finally discovered the second, more serious, infection and Mandela was able to overcome the scary period.
“It took a few days until I felt strong enough to eat,” he told Fortune.
His experience is not unique. With about 75pc of the country's landmass categorised as malaria-endemic, nearly three-quarters of the population is at risk of infection. It is a leading cause of death among children under five, accounting for up to 20pc of fatalities in endemic areas.
However, malaria is making a resurgence with a higher number of cases and deaths than in previous years. Over 2.9 million cases were reported by the Ministry of Health in the last three months alone, representing a 200pc increase compared to the same period in the past few years.
According to Dereje Duguma (MD), state minister of Health, there is no shortage of medicine for malaria except the drug chloroquine. However, this does not mean that treatment is universally accessible.
The supply of malaria medications is not the only challenge facing Ethiopia’s health sector. Malaria cases have surged in several regions.
Hospitals and healthcare centres in the regional state seem to be struggling to keep up with demand. Jinka General Hospital in South Ethiopia Regional State, which serves a vast swath of the southern part of the country, has seen 2,655 confirmed cases in the last three months.
According to Beruktawit Assefa, the medical director, drug supply and blood donations are other issues.
“It’s not been consistent,” said Beruktawit.
The disruption is attributed to both logistical hurdles and financial constraints, as malaria treatment requires an array of medications, blood supplies for severe cases, and preventive tools like mosquito nets and insecticides—resources that are usually in short supply.
Since January, over 7.3 million cases and 1,157 deaths have been reported, according to World Health Organisation (WHO), double when compared to the previous year. Less than a million cases were reported in the year 2019. The WHO report suggests that the result was achieved following years of strong prevention and programs like chemical spraying, net distribution and awareness creation.
However, the resurgence of the disease began to take hold in 2021, driven partly by environmental issues, including climate changes.
State Minister for Health told local media that altered weather patterns have led to increased rainfall, creating more breeding grounds for the mosquitoes that transmit the disease. Warmer temperatures also extend the lifespan of mosquitoes, according to Dereje, allowing them to transmit the parasite over a longer period which has intensified the difficulties of controlling malaria in endemic regions.
The problem is compounded by a growing apathy toward preventative measures. According to health experts, a reduction in vigilance has allowed the mosquito to thrive unchecked.
Hiwot Solomon (MD), a disease prevention lead executive at the Ministry, noted that while bed nets and insecticides remain essential tools in the fight against malaria, many rural areas suffer from inadequate infrastructure to support these interventions.
“Poorly constructed with gaps in the walls and roofs make it difficult to ensure effective protection,” she told Fortune.
Young men, in particular, are the main victims, according to Hiwot, as they often travel long distances for work, sometimes at night when mosquito activity is highest. As cases continue to rise, she warns that the issue will only worsen unless decisive action is taken. Hiwot said the shortage of essential malaria drugs like chloroquine and the difficulties in obtaining them from global suppliers have left many patients without proper treatment.
“We’ve had to rely on alternative treatments, but this is not ideal,” she said, as chloroquine is effective and inexpensive.
Oromia, Amhara, South West Ethiopia regional states account for the majority of the reported cases. Over two million cases were reported by Oromia Health Bureau between January and October, with over 100,000 new cases reported weekly around the borders.
For Tesfaye Kibebew(MD), deputy head of the Bureau, part of the reason for the surge in malaria cases is the region’s vast rural landscape, where people frequently move for work or engage in seasonal labour. These workers often travel to areas with higher malaria transmission, where they are exposed to the disease.
“Cases have tripled than previous years,” said Tesfaye.
With an ongoing conflict in Amhara Regional State, a dramatic rise is seen in malaria cases, with over 80,000 new cases reported in one week.
According to Dametew Lanker, coordinator of the Amhara Regional Health Institute, the resurgence is partly attributed to disruptions in healthcare service and a shortage of necessary equipment, including chemicals and mosquito nets.
"It’s the highest in over a decade," said Damtew.
The increase in cases is not just a matter of more people contracting malaria, but also more severe cases, particularly among vulnerable populations like pregnant women and children. Malaria remains one of the leading causes of death in young children in Ethiopia, accounting for up to 20pc of deaths among children under five. In rural areas, the absence of healthcare facilities and delays in diagnosis exacerbate the risks.
Officials at the Ministry are ramping up efforts to control the spread with a particular focus on increasing the availability of insecticide-treated bed nets and improving the distribution of antimalarial drugs. However, challenges persist. The global malaria vaccine, which has shown promise in trials, remains out of reach for children, who are among the most vulnerable to the disease.
“Application has been filed to receive the vaccine,” said Hiwot, “but so far, we have not been included.”
The federal government is also working to address regional disparities by focusing on the most affected areas. In Gamo Zone, South Ethiopia Regional State, authorities have been working to eliminate mosquito breeding grounds and distribute more mosquito nets to high-risk populations. But, experts argue that community involvement remains crucial.
“We need people to help drain water from stagnant pools and to use bed nets consistently,” said Seifu Wanta, a health bureau officer in Gamo Zone.
Experts indicate the battle against malaria will require a multifaceted approach, combining better healthcare infrastructure, consistent supply chains, and increased community awareness.
Mesfin Alemayehu (MD), a former public health emergency manager in Afar Regional State, notes awareness creation as key to malaria prevention. He urges educating communities about the disease and its prevention, a role he believes extension workers can better fulfil as health education efforts from facilities have weakened. He recommends clearing mosquito breeding grounds and taking prophylactic medication for travelers to high-risk areas. He warned against self-medicating and stressed the need for multiple lab tests to ensure accurate diagnosis.
"It's a common issue in endemic regions," Mesfin told Fortune.
PUBLISHED ON
Nov 16,2024 [ VOL
25 , NO
1281]

View From Arada | Jun 21,2025

Agenda | Oct 06,2024

Fortune News | Oct 08,2022

Fortune News | Jan 03,2025

Fortune News | Aug 18,2024

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
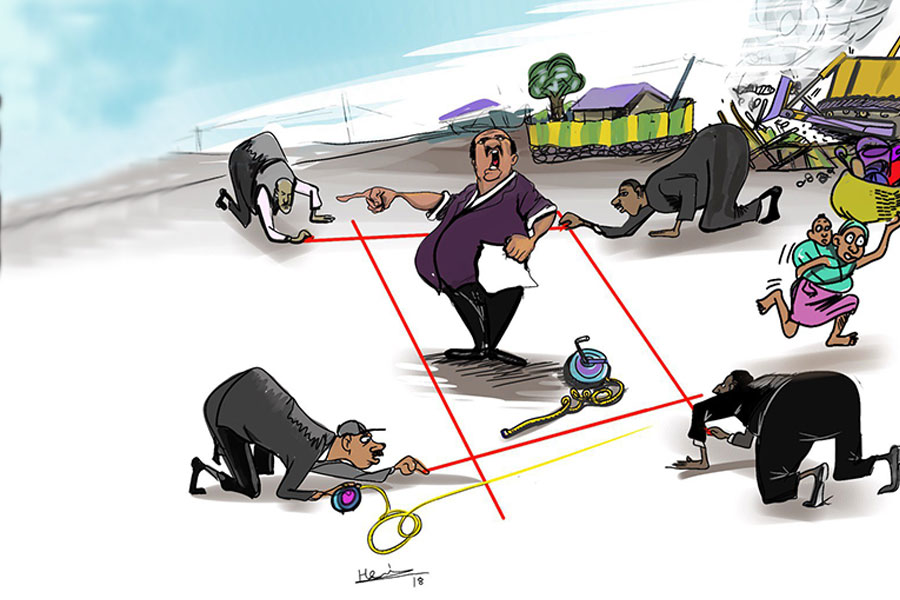
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
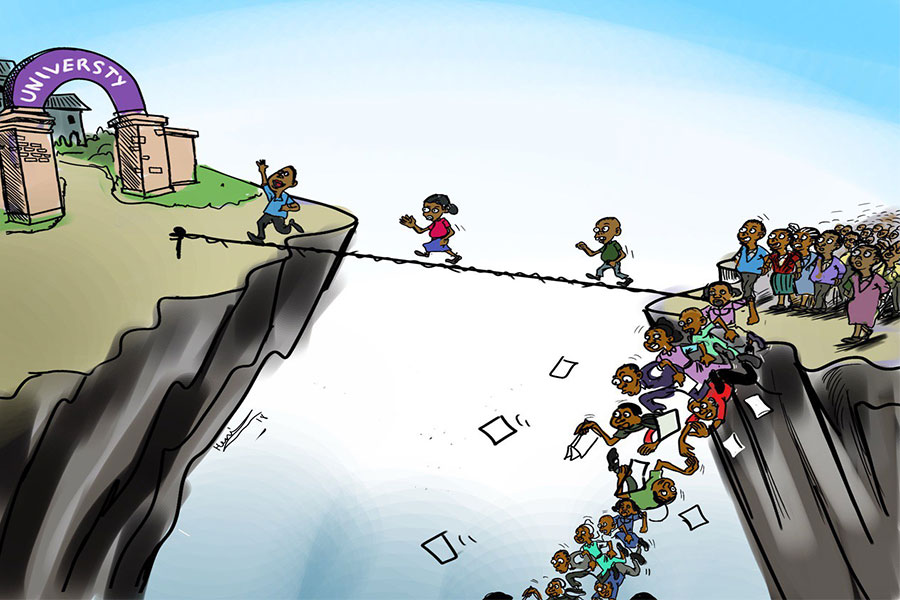
Four years into an experiment with “shock therapy” in education, the national moo...
Sep 20 , 2025
Getachew Reda's return to the national stage was always going to stir attention. Once...