
Covid-19 | Mar 21,2020
Jostling through heavily congested roads worsened by ongoing construction, there is just off to the side an unassuming, depressing, cobblestone alleyway through a cemetery. Several ambulances haphazardly negotiate the route almost every hour on their way to the place that is now a battleground in Ethiopia's precarious fight to contain the deadly virus terrifying the world.
The main entryway to the medical centre was closed for construction. Drivers have to use the gravel road through the cemetery leading to Kotebe St. Gabriel Church before making a turn to the left. Welcome to the Eka Kotebe General Hospital, the largest of two medical facilities the country hopes can help isolate, treat and contain the Novel Coronavirus - aka COVID-19.
A recently built facility, two months ago it was a psychiatric treatment centre with 100 patients. Hurriedly transformed into a place where individuals suspected of having symptoms of the Coronavirus are quarantined and those with confirmed cases are treated, the Hospital has gone through significant reconstruction to make it ready for the battle against the deadly virus.
It was ready when the first confirmed case, a Japanese national who had traveled from West Africa and spent a week traveling around Ethiopia, was identified as acquiring the virus. Doctors and nurses, under the stewardship of Nathanael Bekuretsion (MD), medical director of the Hospital, have been exercising drills for over a month before the arrival of the first patient.
At the age of 28, Nathanael leads a team of medical doctors and nurses, almost all young volunteers. These are professionals on the front line of the indispensable fight against the virus, all of them courageously risking their lives. Many of them have not been home since the first infection case arrived on March 13, 2020, four months after the virus was detected in China.
It is not uncommon to see doctors such as Bruktawit Kidane (MD), 27, sleep on mats inside offices for an average of two or three hours a day to take up one of the three shifts. She is among the 22 medical doctors and 150 nurses attending to the many individuals arriving who are suspected of having the virus. No less than 174 people have visited the Hospital to date, many of them discharged since.
On Friday afternoon, inside the Hospital were eight individuals who have confirmed cases of the Coronavirus, five of whom are foreign nationals, including the oldest woman who is over 80 and the youngest at 33. A British diplomat who traveled from Dubai and tested positive has been quarantined inside the British Embassy, on Comoros St., was confirmed as the ninth case of Coronavirus in Ethiopia.
In the facility at Eka Kotebe are close to 70 individuals, mostly men, suspected of having acquired the virus but waiting for confirmation from laboratory tests regularly conducted at the Ethiopian Public Health Institute (EPHI), off Swaziland St., near St. Paul Hospital. They were kept individually isolated but closely followed by a team of doctors such as Bruktawit and her peers, Bethlehem Tadesse (MD), and Sara Seid (MD). So were Tesfahun Gulelat, 30, and Addis Dejen, 27, on duty in the hospital for days. All young and with few years of experience under their belt as medical doctors, they eat, sleep and work there. Rarely do they venture outside.
Having yet no medicine to administer to cure the virus, these doctors and their aides regularly check the fever level of the patients. They provide them with oxygen support using one of the eight mechanical ventilators, and “regulate ERDS," a medical term to mean checking the fluid levels in the lungs.
“We do all this to boost their immunity,” said the Hospital's Medical Director. “In treating the patients, we are following WHO guidelines and protocols.”
The footprints of WHO and UNICEF can be found throughout the building. Stacks of boxes bearing international brand names filled with medical gear and supplies have been brought in to combat the virus.
WHO: How to protect yourself against COVID-19
Officially christened Novel Coronavirus Disease (COVID-19), it is in the same family of viruses as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS), according to WHO.
Coronavirus mainly attacks cells in the lungs and causes severe pneumonia, according to health findings. Patients with acute cases find it very difficult to breathe because of the fluid that fills their lungs, causing fatalities in some cases. It begins with individuals acquiring the virus from another infected person through particles expelled by coughing or sneezing. Transmission is also likely occurs through handshakes or other forms of physical contact. Entering the body through the eyes, nose or mouth, the initial symptoms are fever, cough and difficulty breathing, according to the World Health Organization (WHO). There are also cases where infected people experience severe headache and digestive problems such as diarrhea.
Officially christened Novel Coronavirus Disease (COVID-19), it is in the same family of viruses as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS), according to WHO. Unlike common coronaviruses that cause mild illness to humans, how COVID-19 first occurred remains debatable. But the first outbreak was detected in an animal market in China, in the Wuhan town of Hubei province, making scientists believe it might have first been transmitted from animals to humans.
The virus has spread fast throughout China since December 2019, forcing Chinese authorities to shut down the entire Wuhan province before it engulfed the entire country. However, COVID-19 has since overwhelmed the world far and beyond China, leading to more than 11,000 deaths around the world. On March 11, the Director-General of WHO, Teodros Adhanom (PhD), declared the virus a global pandemic, after 118,000 people had acquired the infection in 114 countries.
The numbers of infections have kept increasing since then. The countries that have not reported confirmed cases are very few. Only 22 out of 195 countries remain unaffected by the virus that has reached 280,128 on Saturday morning, of whom 11,528 have died. The largest number of deaths have been recorded in Italy where the cost on human life is horrifically high - more than 4,000 as of Saturday morning.
Thankfully, Ethiopia has not recorded any deaths yet. Doctors on the front line of the battle against COVID-19 say almost all individuals with confirmed cases remain stable and strong. None were placed in intensive care, according to the Medical Director.
Under the Ministry of Health, the hospital receives individuals every day suspected of acquiring the virus identified by people working under the Contagious Disease Risk Assessment task force. It is one of the eight groups under the National Emergency Operations Centre (EOC), an interagency crisis management force comprised of policymakers and experts from the Ministry and the Institute.
Usually activated when national emergencies occur, such as this year when cholera outbreaks were reported among internally-displaced people, the task force is often put in a “watch-mood” should there be no catastrophe for a call of duty.
But when the story of COVID-19 menacing the globe surfaced in December, the emergency operations centre was reinforced under the incident management team. Led by Zewdu Assefa, the team has deployed and commands over 100 people, one-forth of which have the responsibility of case management, infection prevention and control, following up on cases, and managing isolation centres. There are at least 40 rapid response teams, each comprised of three members, who receive rumours and tips from the public. Surveillance and follow-up teams, the latter with close to 800 members, are then tasked with monitoring the cases.
Close to 40 ambulance vehicles are deployed and roaming around town picking up individuals with suspected cases of COVID-19. They are brought to Eka Kotebe for now. The Hospital is not nearly close to full capacity, which was inaugurated by Demeke Mekonnen, deputy prime minister, in September 2020. Demeke and Lia Tadesse, minister of Health, were recently back visiting the facility's readiness for the fight against COVID-19, shortly before the arrival of the first individuals.
Although inaugurated recently, the facility has been open since 2017, after consuming close to 200 million Br in construction costs. Hidden away from public visibility and isolated from the cramped neighbourhood, the Hospital was first equipped with 350 beds, half designated for mentally challenged patients. Having two building structures erected alongside each other, the facility incorporates emergency, psychotherapy, rehabilitation, surgery, social and family planning services.
Dawit Kidane (left), CEO of Eka Kotebe General Hospital and Nathanael Bekuretsion (MD), medical director of the Hospital.
It was not easy to transform such a facility designed for a different purpose into an epicentre of the battle against a global menace, according to CEO Dawit Kidane. In preparing it for what would become pandemic, the Hospital was expanded to accommodate between 500 to 550 beds in 400 rooms. Additional structures within the buildings were added to provide space for training, infection prevention, medical services and waste management. Mental health patients receiving care at the hospital were also moved to other locations two weeks ago.
A seven-storey administration bloc is connected with the patients ward through a walkway. On Friday afternoon, doctors and nurses were busy dressing up in full gear of suits, boots, gloves and eye goggles before crossing to the next building where those with confirmed cases were placed in two or three groups. However, individuals with suspected cases are all isolated in 60 separate rooms. On their way back, the health professionals are doing the meticulous task of taking off everything to be destroyed immediately, except the eye goggles.
No one unauthorized is allowed to pass from the window glazed gate of the administrative building to the patients' ward. It is not permissible to observe what goes on inside, but individuals with confirmed cases and suspects, many of whom are foreign nationals, are unhappy with the level of cleaning and standards of the facility. During the first days of their arrival, it was difficult to persuade cleaning staff to enter fully dressed with protective gear to perform the hygiene job, Dawit admitted.
“Things have improved significantly since then,” he told Fortune. “However, managing expectations between the high standard of living they have been familiar with and the state of things here remains a challenge.”
It includes the absence of a hot shower.
But nothing is nearly as challenging to him and his selfless and dedicated staff as the unavailability of potable water, an indispensable provision in any health fight. The Hospital does not get its water supply from the city's water department. For close to three years, a water truck used to provide water twice a week to fill the eight tanks available inside the Hospital. Since the arrival of individuals with COVID-19 cases, however, the frequency of the trucks increased by once a day, filling the 300,000lt capacity to meet a daily consumption of 60,000lt. On weekends, it goes up by 30,000lt.
Although a plan has been activated to drill a water well as a solution, it will not be handy for at least three months.
Medical staff have little to complain about the provision of electric power, although an ongoing road construction project right outside the gate and in the area often brings interruptions. Two generators are on standby, but Dawit wants to have a third generator to guarantee uninterrupted service.
Overworked but determined, the Hospital army believes feeling helpless because of these challenges is not an option.
“We've got to keep on fighting,” said Tsegaye Gebreyes (MD), another young doctor changing into a green gown to take his second shift.
Despite the public's fear and panic, people on the front line such as Dawit and Nathaniel urge authorities to open as many such facilities as fast as possible across the country to absorb what will surely be an increasing number of suspected and confirmed cases. To date, almost all of the cases are individuals who have traveled recently overseas. The situation will become more worrisome when the virus begins to spread throughout the community.
With no cases reported outside of Addis Abeba, Ethiopia's situation is what experts describe as stage one, where individuals who have traveled from countries where the virus is a pandemic are found to be positive. The second stage is when an individual with a positive status transmits it to family members and close friends creating a cluster of cases. The third and most alarming stage is when transmission occurs throughout a small geographic area and expands further. At that point the battle is essentially lost.
The medical staff at Eka Kotebe Hospital want to see the country develop a broader containment strategy before the system gets overwhelmed as in countries around the world where the virus has reached stage three. They warn, “failure will make us pay a huge price.”
For these fighters, well placed to see things from the inside, what is yet to come is entirely unpredictable.
“Society should protect itself from the epidemic,” said Dawit.
PUBLISHED ON
Mar 23,2020 [ VOL
20 , NO
1039]

Covid-19 | Mar 21,2020

Radar | Dec 04,2021

Radar | Dec 25,2021

Life Matters | Aug 14,2021

Life Matters | Jan 29,2022

Fortune News | Mar 28,2020

Photo Gallery | Mar 16,2019
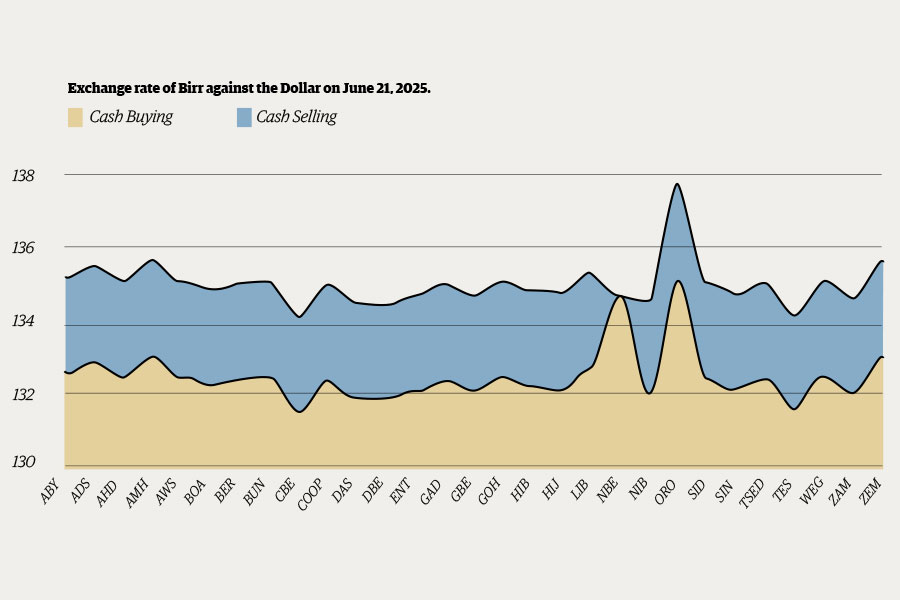
Money Market Watch | Jun 21,2025

Radar | Mar 16,2019

Agenda | Apr 10,2021

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Jul 5 , 2025
Six years ago, Ethiopia was the darling of international liberal commentators. A year...

Jun 28 , 2025
Meseret Damtie, the assertive auditor general, has never been shy about naming names...

Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...

Jun 14 , 2025
Yet again, the Horn of Africa is bracing for trouble. A region already frayed by wars...