
Federal health authorities are piloting a scheme at health facilities to improve service deliveries using limited infrastructure and human resources available at the lowest possible cost. The Ministry of Health (MoH) has identified 38 hospitals where the “system bottlenecks focused reform (SBFR)” programme will be piloted. A dozen of them are in Addis Abeba.
It is the latest initiative in a string of programmes the federal government implements to improve healthcare services.
Ethiopia has been recognised globally for its remarkable gains in the health sector over the two decades, beginning in the early 2000s. The number of health centres has ballooned by almost fivefold to 3,800, and health posts more than doubled to 18,000 over the same period. There are 367 hospitals across the country. With the rapid expansion in medical education facilities, the number of health professionals has grown by a quarter to 210,000. Six percent of them are specialists and general practitioners. Nurses account for a quarter.
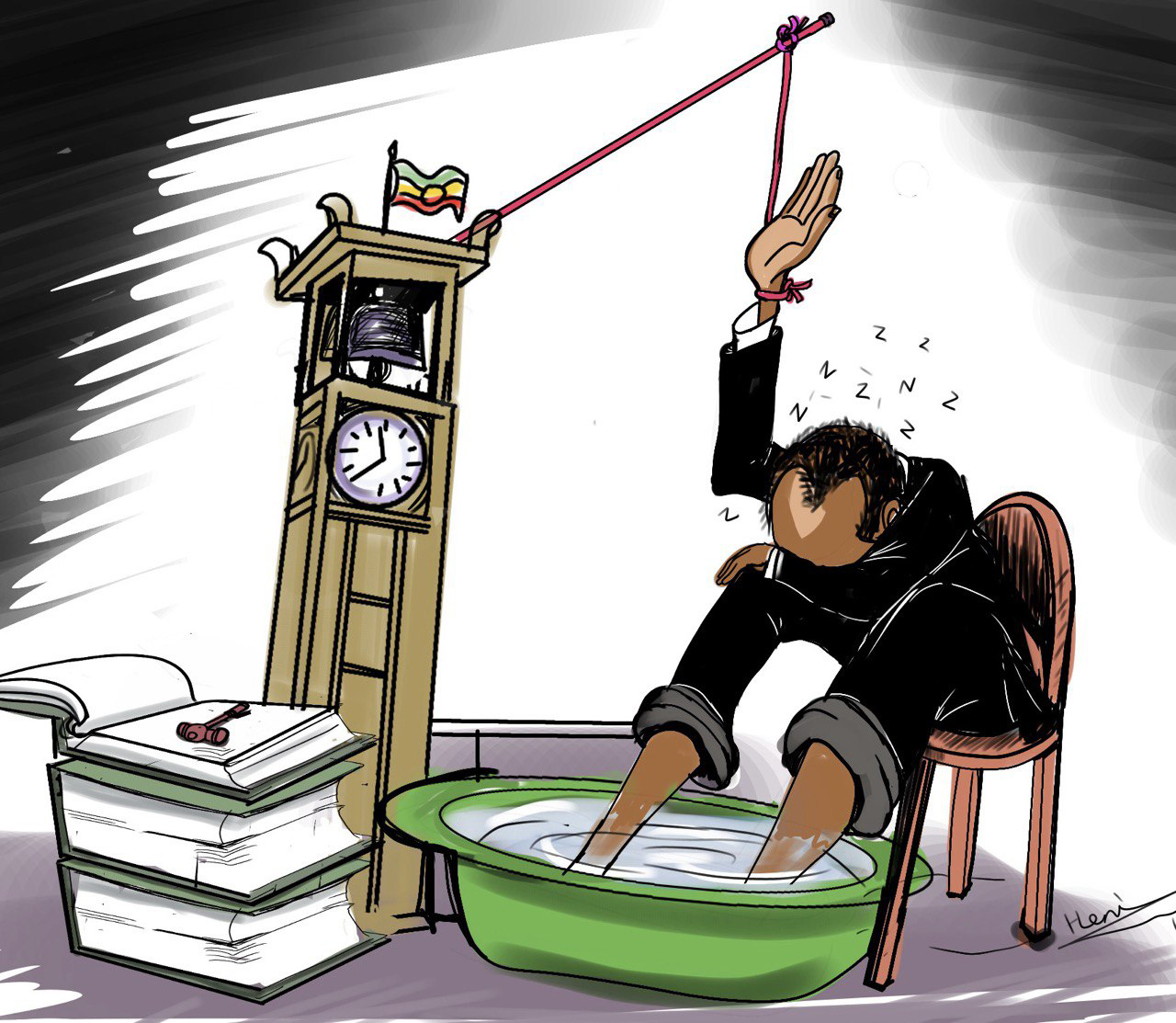
Yet, Ethiopia ranks lower than most African countries in the availability of healthcare personnel, with less than three physicians for every 100,000 people. It is much lower than the World Health Organisation’s (WHO) recommended 10 physicians. According to Ayele Teshome, a state minister for Health, institutions struggle to use the limited number of health professionals and infrastructure fully.
The average national hospital-to-bed occupancy ratio remains less than 60pc. On average, a patient waits more than 35 days for primary surgical care. The State Minister blames the inefficient working system go the inadequacies.
“The inaccessibility of basic and essential hospital services does not necessarily come from the lack of resources,” said Ayele. “Poor data quality management and lack of integration contribute to the inefficiency.”
The authorities say that improving the system with innovations designed to utilise available resources is crucial to improving service delivery.
Jimma University Medical Centre, 352Km southwest of Addis Abeba, is among the health institutions chosen for the scheme’s piloting.
Emebet Dage (MD), director of the inpatient care unit, saw how 120 specialists and physicians struggle to serve in the health facility that receives 16,000 inpatients and 220,000 outpatients annually. It also treats 12,000 emergency cases each year.
Its administrators have set up one-stop consultation services to better avail medical specialists to patients, supervised by a senior physician. The Centre has established a health literacy unit to follow up and consult patients who need follow-up care. A general practitioner leads the unit. The Hospital is also preparing five duty rooms to accommodate the needs of the physicians, Emebet disclosed.
The scheme's major components are the automation of electronic medical record systems and the digitisation of clinical and non-clinical services.
Yekatit 12 Hospital Medical College is part of the pilot. It has used an electronic medical record system for three years, developed for 10 million Br. It registers basic medical information about diagnoses, treatment and lab results.
Medical professionals say the digital registry is a considerable improvement on the manual record system that allows easy access to comprehensive patient information. Close to 124 medical specialists work at the Hospital.
“It makes it easy to search and update patient data and assign medical doctors,” said Alemu Kibret (MD), administrative and development vice provost.
Established in 1923, Yekatit 12 Hospital provides medical services to 360,000 patients annually.
Alemu says there is a shortage of specialists, including anaesthiologists, and plastic and trauma surgeons.
Although emergency and critical care services are essential in the health system, data reveals limited access to intensive care units (ICU). The annual ICU mortality rate is over 25pc, significantly higher than the global average of 18.2pc. Reducing the mortality rate requires addressing inefficiency, system disintegration, poor practices, and a lack of proper accountability mechanisms, according to the State Minister.
Health officials plan to run the pilot for a year before taking it national.
PUBLISHED ON
Sep 10,2022 [ VOL
23 , NO
1167]

Radar | Feb 19,2022

Fortune News | Aug 05,2023

Fortune News | Apr 17,2020

Commentaries | Feb 10,2024

Fortune News | Nov 11,2023

Fortune News | Aug 06,2022

Radar | Oct 23,2021

Agenda | Sep 21,2019

Fortune News | Sep 18,2021

Fortune News | Jan 25,2020

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Jul 12 , 2025
Political leaders and their policy advisors often promise great leaps forward, yet th...

Jul 5 , 2025
Six years ago, Ethiopia was the darling of international liberal commentators. A year...

Jun 28 , 2025
Meseret Damtie, the assertive auditor general, has never been shy about naming names...

Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...