
Viewpoints | Jan 07,2023
Minister of Health Lia Tadesse (MD) has displayed her ambition of rolling out a three-year investment and development roadmap, targeting the rehabilitation of health facilities in regions ravaged by conflicts and wars. With an estimated budget of 16.3 billion dollars, her ambition marks a significant move towards addressing the country's pressing health issues, including rising non-communicable diseases, injuries, and malnutrition, against a backdrop of diminished public health emergency response capacity.
The investment plan with nine targets is critical for Ethiopia, as the country contends with alarming health statistics exacerbated by recent conflicts. A substantial portion of the funding, over 50pc, is expected to come from development partners, while the federal government treasury is to share 19pc, and public-private partnerships are slated to cover 11pc.
This comes as donor contributions have shown a decline, plummeting by up to 241pc over the past two years, primarily due to the conflict. The drop starkly contrasts with the annual pledges of 150 million dollars during the implementation of the second edition of the health transformation plan under the Sustainable Development Goals (SDGs).
Central to the plan, a.k.a Health Sector Development & Investment Plan (HSDIP), is the post-conflict recovery phase, which prioritises restoring damaged health facilities and mobilising a critical health workforce. The plan also emphasizes the importance of providing psychosocial support in zones experiencing wars and ensuring the availability of essential services like water, sanitation, reproductive, neonatal, and nutrition services across all health facilities.
The two-year conflict in the Tigray Regional State and neighbouring states has had a devastating impact on the country's healthcare infrastructure. At its peak, the conflict led to the internal displacement of nearly 5.8 million people in Tigray, Amhara and Afar regional states. The Ministry of Health reported that over 76 hospitals and thousands of health facilities were destroyed, with total damages exceeding 1.4 billion dollars. The destruction has left the health system vulnerable and struggling to cope with epidemics of cholera, measles, meningitis, and acute respiratory infections.
Abraha Gebregziabher (MD), the medical director of Ayder Hospital in Meqelle, expressed the urgent need for government assistance. The Hospital, serving nearly eight million people in the regional state, is overwhelmed with patient influx and limited by inadequate capacity. He noted the dire state of the Hospital's infrastructure and equipment, with crucial facilities like a chemotherapy machine lying unused due to the conflict.
"Several corridors are permanently dark," he told Fortune of the ageing electrical system.
Despite these challenges, Ayder Hospital, with 200 specialist doctors and nearly 2,300 staff, provided 300,000 outpatient services last year. A significant number of these patients were malnourished, demanding care beyond the capabilities of lower-tier medical facilities in the regional state. The Medical Director revealed that while therapeutic foods are in better supply, there is a constant shortage of anti-infection medication for the scores of malnourished patients who come to the hospital.
"It's heartbreaking to tell patients to look for treatment elsewhere," Abraha said. "Most months, we're out of supply".
The recent announcement by USAID to resume food aid throughout Ethiopia offers a glimmer of hope in addressing the severe food insecurity affecting the regional state. However, the health sector's crises are compounded by Ethiopia's low per capita health expenditure, which is less than half of the World Health Organization's recommended 86 dollars. Out-of-pocket health expenses constitute 30pc of the total health expenditure.
The Ethiopian Health Insurance Agency (EHIA), in its 12th year, has made strides in expanding medical care, now covering over 56 million beneficiaries under the Community-Based Health Insurance (CBHI) scheme. Tesfaye Worku, director of the Agency, emphasised the need for long-term commitments, including rigorous inspections and restorations of health facilities, before implementing the scheme in conflict-affected regions.
"Affordable health care is the ultimate goal," Tesfaye told Fortune. "It requires long-term commitments."
Despite CBHI covering around 87pc of weredas in the country, challenges remain, including fragmented pooling and limited access for the needy. The social health insurance for formally employed citizens is still in limbo.
Another strategic objective is the reduction of child stunting from 39pc to 25pc.
Hiwot Darsene, chairwoman of a National Food & Nutrition technical committee under the Ministry, spoke of the importance of rehabilitating health facilities in post-conflict regions as a key component of the national health and nutrition strategy. New approaches, including humanitarian direct cash transfers, mobile health services, and public-private partnerships, are planned to improve health access in remote areas.
Hiwot believes there is a need for changes in agricultural methods, private sector involvement in food supply chains, and effective regulation by the Ministry to address malnutrition. The Health Ministry enforces mandatory mineral enrichment in edible oil and flour products, as global market disruptions in food supply, severe drought, and internal politics exacerbate malnutrition cases.
However, the reliance on donor funding, which accounts for nearly all of Ethiopia's acute malnutrition rehabilitation programs, posed a risk to the sustainability of these initiatives.
"The decline in donor funding has an indirect impact," she said.
Getasew Amare, a health economist at the University of Gonder, warns that dependency on donor funding is unsustainable in the current global political climate. He advocates for financial mobilisation strategies to be revised, including social health insurance schemes and health expenditure mobilisation from the private sector.
Getasew commended Minister Lia's focus on acute malnutrition and post-conflict rehabilitation of health facilities but cautioned her that this approach largely addressed the consequences rather than the root causes. According to Getasew, malnutrition in early childhood can have lasting impacts on cognitive development and workforce performance, stressing the urgency for effective and sustainable solutions in the health sector.
"Investments in nutrition have the highest rates of return," Getasew told Fortune, "The malnourished of today will tragically become dependents tomorrow."
PUBLISHED ON
Nov 25,2023 [ VOL
24 , NO
1230]

Viewpoints | Jan 07,2023

Fortune News | Jun 01,2019

Fortune News | Nov 30,2019

Radar | Feb 25,2023

Viewpoints | Sep 23,2023

Addis Fortune | May 04,2024

Fortune News | Oct 31,2020

Radar |

Radar | Nov 05,2022

My Opinion | Feb 11,2023

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Jun 28 , 2025
Meseret Damtie, the assertive auditor general, has never been shy about naming names...

Jun 21 , 2025
A well-worn adage says, “Budget is not destiny, but it is direction.” Examining t...

Jun 14 , 2025
Yet again, the Horn of Africa is bracing for trouble. A region already frayed by wars...
Jun 7 , 2025
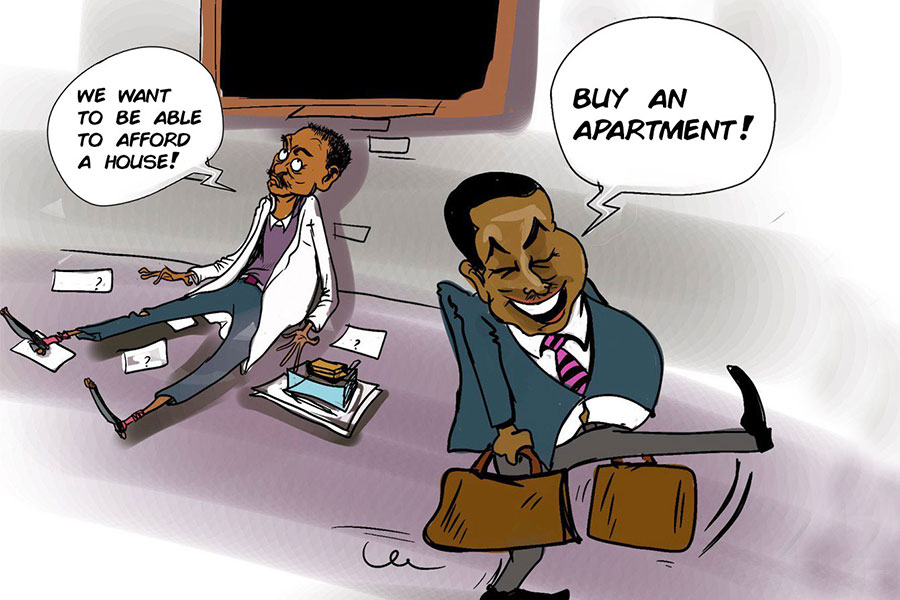
Few promises shine brighter in Addis Abeba than the pledge of a roof for every family...