
Fortune News | May 31,2020
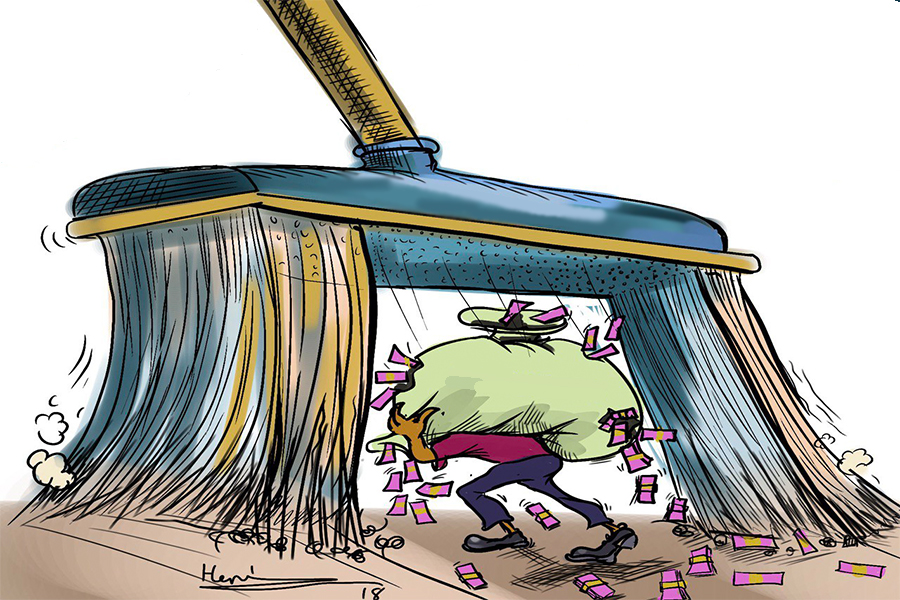
Hospital administrators and directors of the federal agency supplying pharmaceuticals and medical equipment to public health institutions are at odds over a new payment modality.
Heads of the Ethiopian Pharmaceuticals Supply Agency (EPSA) rolled out a payment arrangement for public hospitals to pay half the cost of drugs and medical equipment in advance. Reestablished in 2007, the agency supplies 1,200 medicines and medical equipment to 5,000 public health institutions on a credit and cash basis. Thirty-two of these institutions are hospitals.
Under the administration of Abdulkadir Gelgelo (MD), the agency attempts to rejuvenate the national drug supply chain by expanding its sources of revenue.
Last year, the agency supplied drugs and equipment valued at 51 billion Br. However, the supply is hardly sufficient to meet demand. The new arrangement responds to the crippling drug and medical supply shortages that have gripped public health centres.
The Agency demands health centres buy drugs on credit and settle payments within two months of receiving the supplies. However, many hardly adhered to the rules and paid their debts on time, according to Solomon Nigussie, deputy director. Receivables owed to the Agency increased by 400 million Br over the past two months. Health centres collectively owe it 1.2 billion Br.
“Occasionally, hospitals refuse to pay for drugs and medical equipment after placing orders,” said Solomon.
Hospital administrators retorted that the new payment arrangement is detrimental to boosting drug supply and meeting the growing demand for medication. Despite dwindling inventory, health centres cannot procure drugs and equipment due to budgetary constraints. Although public health centres are required to maintain two months’ supplies in their inventories, most hospitals barely keep two weeks of stock.
The shortage is visible at St. Peter's TB Specialized Hospital.
The consensus among hospital administrators is advance payment should be 30pc of the cost, according to Chale Molesa, a representative of the director of pharmacy.
“The budget allocated to drug procurement falls short of the need,” he told Fortune.
St. Peter Hospital’s administrators received a 45 million Br budget for drug procurement last year. It's administrators say it is insufficient. It was not disbursed on time. Ahemedine Seid, director of pharmacy at Hawassa University Comprehensive Specialized Hospital, echoed similar concerns.
“The budget disbursement doesn’t align with the monthly demand for drugs,” he said.
With 480 beds, the Hospital admits over 11,000 patients annually and treats 117,000 outpatients. Its administrators had proposed a 73 million Br budget for drug procurements this year. They received approval for 33pc of their need. The Hospital receives two million Birr a month for drug procurements.
Declining external loan disbursements and increasing global prices for essential commodities such as fuel, fertiliser, and wheat have forced federal officials to cut public expenditures this year. The decision has directly impacted public health institutions operating under the supervision of the Ministry of Health (MoH). Although they had submitted a 13.2 billion Br budget, finance authorities approved two-thirds of this.
Finance Minister Ahmed Shide and his deputies advised health officials and hospital administrators to cover the balance independently, generating revenues through increasing medical bills.
Ahemedine says Hawassa University Hospital plans to generate 40 million Br from billing patients.
Budget allocations are not based on actual demands, says Dawit Teshome, lecturer of pharmaceutical supply chain management at Tikur Anbessa Medical School.
“However, the Agency could have safeguarded itself if hospitals fail to pay, buying insurance policies,” he said.
Federal authorities have noted the tensions between the agency’s officials and hospitals’ administrators over drug supplies. They have acknowledged the constraints the hospitals faced.
“We’re discussing the issue with finance officials,” said Dereje Duguma (MD), a state minister for Health.
The State Minister believes the pre-financing modalities were introduced after considering the experiences of African countries that have implemented similar procedures, such as Kenya.
“Most hospitals can pay half the cost upfront,” said State Minister Dereje.
The rapid erosion of the Birr against major currencies is driving up the cost of importing drugs and equipment. The agency buys over 90pc of its drugs from international suppliers. It used to source a quarter of its supplies from local manufacturers. However, the share has dropped to less than 10pc. Strapped on forex, local pharmaceuticals are operating at a fraction of capacity.
Under the banner of the Pharmaceutical Manufacturers Association, an industry lobby group representing 17 members, local manufacturers placed applications for 15 million dollars in letters of credit to import inputs. Inadequate financing remains the most pressing problem in the pharmaceutical supply chain.
Similar to hospitals, the agency, which depends on a revolving drug fund, is also struggling with insufficient funding. It generates revenues from donors’ contributions and the 10pc service fee it charges.
Despite the pushback from administrators of hospitals, the agency is “committed to implementing the new payment arrangement to ensure a sustainable supply of drugs,” says Solomon.
PUBLISHED ON
Sep 18,2022 [ VOL
23 , NO
1168]

Fortune News | May 31,2020

Radar | Sep 28,2019

Radar | Oct 16,2021

Radar | Dec 21,2019

Radar | Feb 23,2019

Fortune News | Apr 09,2022

Fortune News | Jan 11,2020

Radar | May 13,2023

Sponsored Contents | Jan 31,2022

Fortune News | May 11,2019

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Oct 25 , 2025
The regulatory machinery is on overdrive. In only two years, no fewer than 35 new pro...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...