
View From Arada | Aug 20,2022
May 31 , 2020
By Michael Getachew ( Digital medicine coordinator for Johns Hopkins University and Saint Paul's Hospital Millennium Medical College. )
Since the first few months of the year, the focus of much of the healthcare apparatus in Ethiopia has been on the Novel Coronavirus (COVID-19) pandemic. This is understandable since the virus poses an unexpected threat and requires immediate mobilisation of resources and personnel.
With time, however, this pandemic will pass, and Ethiopia will remain deficient in other aspects of its public health goals. This is also the case for vaccinations, which we should not lose sight of.
Even after two decades of vast improvement, the rates of infant and under-five mortality in Ethiopia are still among the highest in the world, while Diarrhoeal diseases and vaccine-preventable diseases (VPDs), paired with malnutrition, still cause a majority of childhood deaths in Ethiopia.
Immunisation coverage has not met public health targets, and, without renewed focus, the nation may fall further behind. Improvements in the vaccine delivery pipeline ought to be sustained to protect Ethiopia’s children from preventable suffering. Most notably, achievements in cold chain infrastructure must be maintained to hold onto the gains made in previous years.
Cold chain management describes the recommended procedures and technology for maintaining storage temperatures of vaccines at every stage between the lab and the patient. Otherwise, vaccines lose their potency. Cold chain failure could result in major outbreaks of VPDs.
The primary constraints on vaccination in the Ethiopian context are a lack of top-down supervision, high drop-out rates (meaning children fail to receive follow-up doses of their vaccination regimen), an insufficient number of trained health workers and inadequate supplies like cold chain equipment, according to the most recent review of Ethiopia’s Extended Programme of Immunisation (EPI), its main vehicle for carrying out the expansion of childhood vaccination.
Diphtheria, measles, pertussis, tetanus, polio and tuberculosis are the six VPDs included in the EPI programme. Additionally, there are long-term plans to introduce more vaccines, such as Hepatitis B and Hemophilus Influenzae Type B.
The focus of many medical professionals when it comes to vaccination is mostly on delivery, accessibility and public awareness. But due to social distancing and the state of emergency, including policies that restrict movement, it has become more difficult to carry out vaccination services for those in more remote sections of the country.
In Addis Abeba, vaccinations in most case are available in public health clinics in every district of the city. But for some, especially in the rural areas, it can be challenging to reach those targeted groups because of lack of transportation or limited access to certain areas of the country. Another obstacle or challenge is the required refrigeration system that the drugs require, without which vaccines become useless.
Another barrier at the moment comes to the social messaging campaigns that are paramount to creating awareness among parents about the need to vaccinate their young children. Due to COVID-19, these messaging campaigns, an integral part of the overall public health strategy, are not being carried out.
In normal times, local members of immunisation outreach teams distribute information about VPDs through theatre and dance routines on market days, at religious meetings, at schools, and at regular women’s group meetings. But with ongoing lockdowns and social distancing decrees, many of these events have been cancelled for the time being, leaving the messaging campaigns in limbo.
This is damaging to the country's overall public health goals because advocacy helps to gain the commitment of decision-makers and build community support for immunisation. This is why the Ministry of Health has made health structures incorporate health messaging in all its health programs.
One additional barrier to immunisation that predates the COVID-19 pandemic is the lack of trained human resources at all levels. Until recently, the situation was improving, though a high attrition rate remains a pressing issue. The shortage of trained personnel is most acute at the health facility level in rural areas that only have a few health workers in charge of maternal and child health services. Due to the pandemic, more staff would need to be diverted to fight the virus.
All is not lost. In fact, all available information points to the government reigniting the Reaching Every District (RED) strategy once the pandemic dies down. This strategy involves the inclusion of lower-level staff in tactical planning and, in turn, offering them more training. RED also provides quality and recurrent supervision, which is key to achieving high vaccination coverage and is needed to counteract the effects of heavy staff turnover. The RED plan also calls for reaching all qebelesat least four times a year in remote regions with a large number of unvaccinated children using health extension workers.
The challenges to vaccination the COVID-19 pandemic poses could have dire consequences. But with more imagination and perseverance, they are not insurmountable.
PUBLISHED ON
May 31,2020 [ VOL
21 , NO
1049]

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Oct 25 , 2025
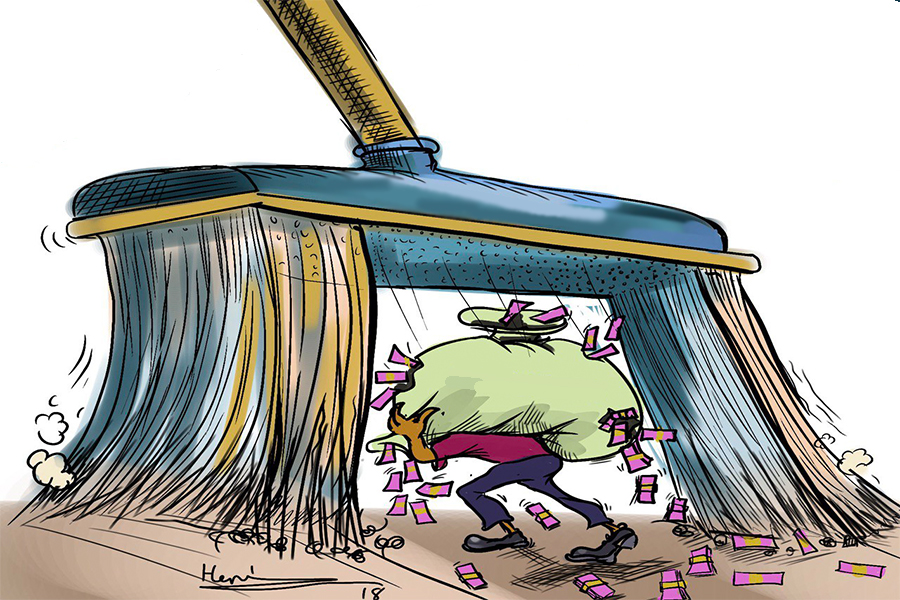
The regulatory machinery is on overdrive. In only two years, no fewer than 35 new pro...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...
Oct 4 , 2025
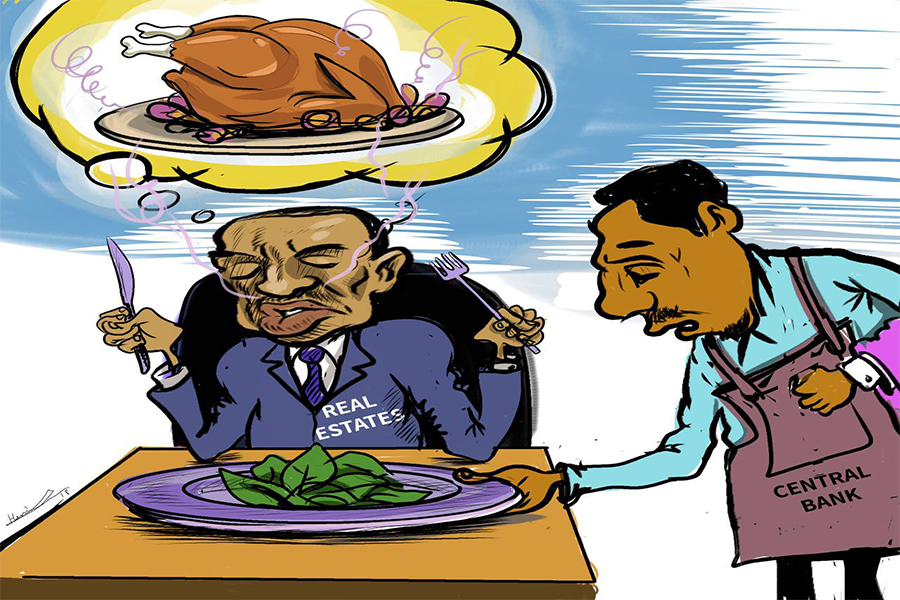
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...