
My Opinion | Aug 10,2024
On a rainy afternoon, Almaz Teshome, draped in yellow and black, walked through the 8th-floor hallway of Tikur Anbessa Specialized Hospital (TASH). She had just visited her 30-year-old son, newly diagnosed with type II diabetes. Almaz, who has battled diabetes herself for 30 years, had been relying on insulin for treatment. However, over the past six months, the insulin she bought from Zewditu Hospital had only worsened her condition.
"I felt worse every time I took it," Almaz said.
She recalls how the medication left her feeling heavy and warm, with trembling hands and debilitating headaches. A beneficiary of Community-based Health Insurance (CBHI), Almaz, 65, depends on her children for support. She ultimately had to stop the medication when she could no longer bear the side effects.
Almaz noted that the new insulin, which sold for 250 Br, differed in appearance—it was more transparent and watery compared to the thicker, milky texture she had been accustomed to for 20 years. When physicians could not offer a clear explanation for her concern, she considered buying medicine directly from traders, despite the cost being three times higher.
"It's more than I can afford," she said. "I don't know what to do."
Her experience is not an isolated case. Insiders at Tikur Anbessa have revealed a surge in complaints from patients, citing that insulin and chemotherapy drugs over the past year were not working effectively.
Regular treatment receivers including diabetic patients voiced concerns to their association. The Ethiopian Diabetics Association (EDA) collaborates with health centres through its 76 branches, providing insulin vials, oral tablets, and training for health professionals.
Ermias G. Mariam, vice president of the 40-year-old Association, acknowledged that there have been complaints about potential product defects among 20 patients recently. However, he believes that out of 90,000 members, the numbers do not warrant that a crisis is looming. He said the issues some patients are experiencing with the new insulin could be related to improper administration.
"Even though there is a problem, we will find a solution soon," he said.
Conducted by researchers from the universities of Bahir Dar and Gonder, a recent review analysed 27 studies and reviews across sub-Sahara Africa, finding that nearly 22pc of 7,508 medicine samples failed at least one quality test. These were confirmed to be substandard, falsified, unlicensed, unregistered medicines posing substantial risks to public health.
Biset Asrade (MD), a pharmacology lecturer at Bahir Dar University and one of the researchers involved in the study, noted that the high demand for certain medicines opens the door for illicit products, with supply chains in Ethiopia being complex, inefficient, and fragmented. He stressed the need to strengthen supply chains across Africa by improving infrastructure, logistics, and surveillance systems.
"It's a major public health concern," he warned.
The prevalence of unregistered medicines is even higher, averaging 34.6pc, with antibiotics, antimalarials, and antihypertensives making up 44.6pc, 15.6pc, and 16.3pc of these cases, respectively. Contributing factors include poor market regulation, free trade zones, inadequate registration, high demand, and low importation standards.
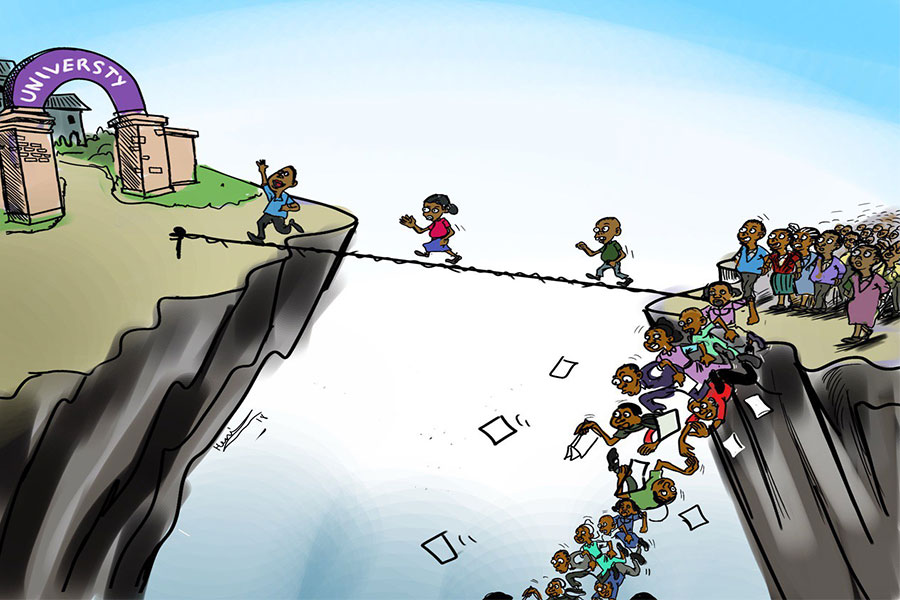
More than 85pc of Ethiopia’s pharmaceutical market is met through imports, with India (22pc), the Netherlands (20pc), and Belgium (13pc) being the largest source countries. With over 380 private importers and nearly 500 wholesalers involved in the sector, the Ethiopian Pharmaceuticals Supply Service (EPSS) is the largest pharmaceutical products buyer with 85pc supply share. It distributed over 1,000 types of drugs and medical equipment worth 17 billion Br last year to more than 5,000 public health institutions.
Tariku Belachew, deputy head of EPSS, emphasised the urgent need to enhance the integrated monitoring system to meet growing demands.
"We need to work closely with health institutions," he said, underscoring the importance of monitoring adverse drug effects once they reach consumers.
Tikur Anbessa, serving over 800,000 patients annually, procures medicines worth over 210 million Br yearly from EPSS. The Hospital’s pharmacy director, Demis Gezahegn, reported that technical product deficits occur when the active pharmaceutical ingredient falls below the standard of 90pc, when tablets are brittle, or when medications are unlabelled.
"Some medicines misrepresent their identity, composition, or source," Demis said, adding that antibiotics and psychotic medicines require the most caution. He stressed the need to strengthen supply chains across Africa by improving infrastructure, logistics, and surveillance systems.
So far, no official complaints have been filed with the Ethiopian Food and Drug Authority (EFDA). The Authority has received only 1,600 pharmacovigilance reports out of the planned 11,000, representing just 28.9pc of the expected Adverse Drug Experience reports.
Responsible for regulating such issues, the Authority has been proactive in warning health institutions against prescribing potentially harmful over-the-counter medicines. According to Fozia Mohammed, head of the Authority’s inspection desk, the dangers posed by smuggled products that bypass inspections are the culprit.
"The illicit market could be a problem," she said, emphasizing the role of inspections in preventing unregulated chemicals from entering the country.
However, she acknowledged that there were no reports from hospitals about adverse reactions to medicines. The Authority screens the nearly 2,000 importers, wholesalers and manufacturers. A half-year report for the last fiscal year quantified that medicines worth over 107 million Br were disposed of for being unauthorised, outdated, substandard, and illegally imported or stocked.
Heran Gerba, director of the Authority, noted that many hospitals fail to submit timely reports, indicating that weak follow-up and delays in reporting are ongoing challenges, despite eight pharmacovigilance centres in university hospitals.
"There is a lack of awareness in reporting procedures," she said.
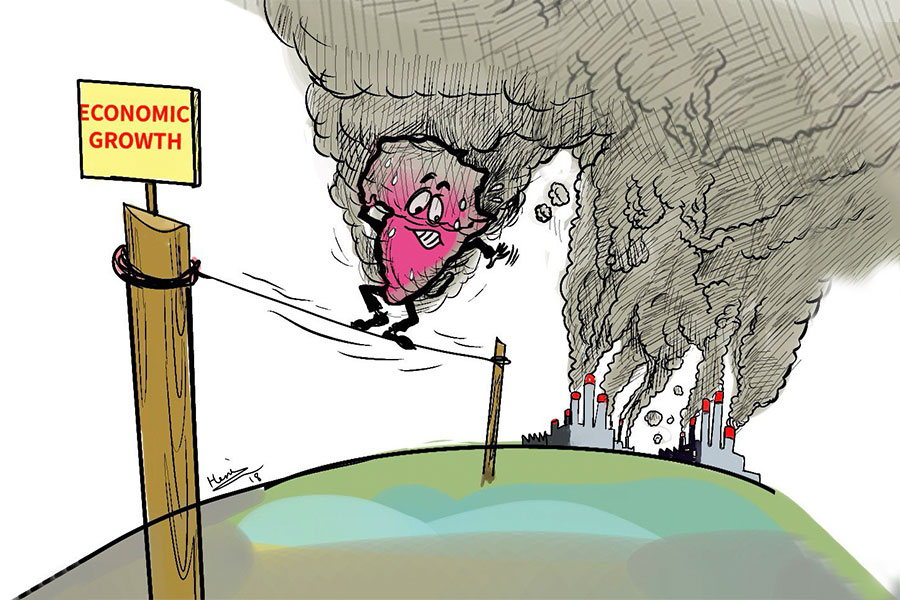
The global trade in counterfeit pharmaceuticals is valued at up to 4.4 billion dollars—representing 0.84pc of total worldwide imports, causing up to half a million deaths a year in sub-Sahara Africa alone.
Forex shortages and global supply chain disruptions have hindered progress in the pharmaceutical industry lately. Despite foreign investment accounting for up to 40pc of total pharmaceutical investments three years ago, manufacturers’ capacity has dropped to just five percent, according to the lobby group representing them.
Yohannes Fisehha, deputy general manager of Addis Pharmaceutical Factory, stated that pharmaceutical materials are primarily imported from India, Europe, and China. The factory supplies half of its capacity to EPSS. Yohannes acknowledged the industry's efforts to comply with international standards but highlighted the financial burdens of compliance, with foreign currency being a significant barrier. He expressed confidence in the quality of his raw materials, which undergo rigorous testing before processing.
"There might be overlooked items," he said, adding that manufacturers undergo proper analysis, and any defective medicines are discarded.
The illicit pharmaceutical market not only jeopardizes treatment but also contributes to the development of drug-resistant strains, reducing the efficacy of legitimate medicines. This increases costs for patients and healthcare systems and damages the reputation of healthcare facilities.
The most frequently counterfeited and falsified medicines in developing countries include those used to treat life-threatening conditions such as cancer, malaria, tuberculosis, and HIV/AIDS. The research warns that this problem is escalating, with an increasing number of counterfeit and falsified medicines flooding the market.
One of the 14 health centres in Addis Ketema District, which serves over 129,000 patients annually, has implemented control and reporting mechanisms for defective medicines. According to Fikadu Worku, the managing director, they faced incidents last year where defective Amoxicillin pills negatively impacted patients' health. He noted that supply shortages from the EPSS sometimes force them to turn to wholesalers and importers after floating bids.
"There are shortages," Fikadu said.
PUBLISHED ON
Aug 11,2024 [ VOL
25 , NO
1267]

My Opinion | Aug 10,2024

Fortune News | Aug 02,2025

Fortune News | Jul 13,2024

Advertorials | Nov 15,2023

Obituary | Jan 28,2023

Fortune News | May 16,2020

Fortune News | May 27,2023

In-Picture | Jul 28,2024
Fortune News | Nov 03,2024


Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
Four years into an experiment with “shock therapy” in education, the national moo...
Sep 20 , 2025
Getachew Reda's return to the national stage was always going to stir attention. Once...
Sep 13 , 2025
At its launch in Nairobi two years ago, the Africa Climate Summit was billed as the f...