
Fortune News | Jan 07,2024
Behind the nondescript facade of a drop-in centre in Addis Abeba, a quiet struggle unfolds nightly. Among those seeking refuge is a 25-year-old sex worker, driven by financial hardship from waitress to the streets. The centre, offering essential services like showers, meals, and STI tests, also provides a crucial lifeline: condoms. Yet, a severe shortage looms, leaving women to fend for themselves in a perilous gamble with their health. The bi-weekly allotment of eight condom packets from Population Services International (PSI) Ethiopia barely scratches the surface of their needs.
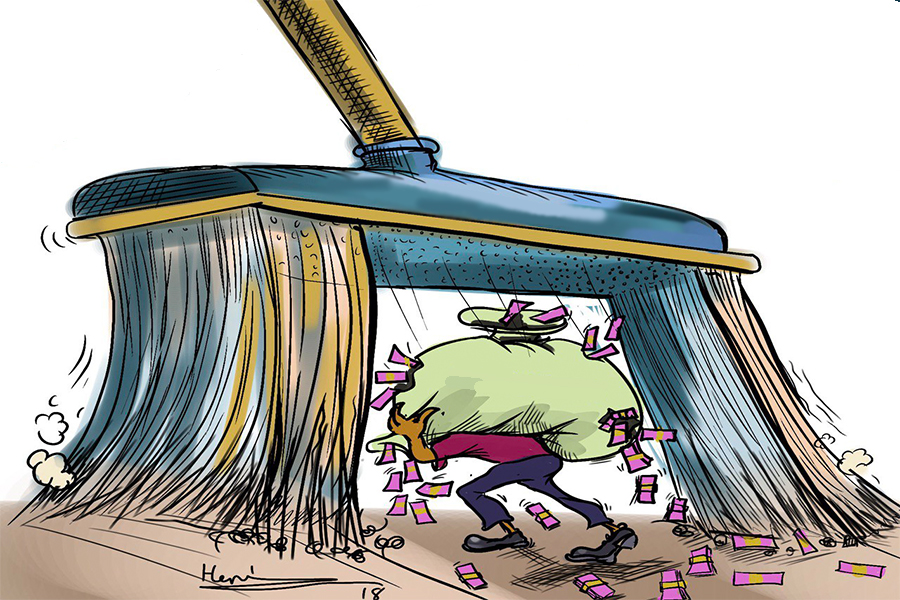
Ironically, this scarcity persists despite Ethiopia’s soaring HIV infection rates and dwindling funds from international donors. The Ethiopian Pharmaceutical Supply Services (EPSS) and NGOs like DKT International and PSI Ethiopia scramble to cover an annual demand of 250 million condoms but only manage to provide about 100 million. Free condom distributions, once common in universities and public spaces, are now a rarity. Health centres have cut down their giveaways drastically, capping them at three packs per person, under the pretext of preventing resale.
Health officials blame the restrictions on alleged abuse. The heads of the pharmaceutical supply services at the Addis Abeba Health Bureau insist the caps are necessary to curb resale. However, health centre managers tell a different tale of overwhelming reliance on donor support as government supplies fall drastically short. They recount receiving a fraction of requested supplies from EPSS, with donors stepping in to fill the gap. Yet, the restrictions remain, ostensibly to ensure wider access.
The Ministry of Health acknowledges the supply shock post-COVID-19, justifying its focus on high-risk groups like sex workers and adolescent girls. Those in charge of HIV prevention argue that strategic prioritisation is essential amid declining global funding. The targeted approach, however, leaves institutions like Addis Abeba Science & Technology University in the lurch, exacerbating sexually transmitted infections (STI) and unwanted pregnancy cases among students. A public health officer at the University lamented the rising demand for condoms he cannot meet.
Compounding the crisis is the stark irony of rising condom prices amidst the shortage. Pharmacists are forced to add markups to already inflated wholesale prices, pushing condoms further out of reach for many priced between 40 Br and 60 Br. While DKT Ethiopia attempts to respond by selling at subsidised rates, the convoluted procurement process and customs delays only add to the woes. Its managers urge health officials to intervene in price caps to bridge the gap.
Ethiopia’s battle against HIV/AIDS poignantly reflects global funding disparities and local inefficiencies. The quality of imported condoms is another concern, with a portion failing to meet standards and being destroyed or returned. Officials of the Ethiopian Food & Drug Authority, a federal agency, recall the sharp decline in quality this year, a grim reminder of the complexities plaguing public health efforts. The fight for a healthier future continues, marred by irony and systemic flaws.
You can read the full story here
PUBLISHED ON
May 18,2024 [ VOL
25 , NO
1255]

Fortune News | Jan 07,2024

Commentaries | Jan 14,2023

Fortune News | Oct 13, 2024
Advertorials | Jun 12,2023

Fortune News | Jun 18,2022

Radar | Aug 21,2023

Fortune News | Nov 05,2022

Agenda | Nov 27,2022

Verbatim | May 31,2025

Viewpoints | May 11,2024

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...
Oct 25 , 2025
The regulatory machinery is on overdrive. In only two years, no fewer than 35 new pro...

Oct 18 , 2025
The political establishment, notably the ruling party and its top brass, has become p...

Oct 11 , 2025
Ladislas Farago, a roving Associated Press (AP) correspondent, arrived in Ethiopia in...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...