
Radar | Apr 19,2025
Discarded green camouflage military garb, distinct from the digital pattern of the Ethiopian National Defense Force, lies among the items strewn over the ground behind Frewoini Primary Hospital, two hours’ drive from Meqelle, capital of Tigray Regional State.
Two broken wheelchairs, an assortment of discarded documents, and scraps of garbage make up the rest of the effects on the floor of the Hospital where locals claim the Eritrean military had been camped out for over a month in late November, just weeks following the outbreak of war in the Regional State. Military uniforms that seem to belong to Eritrean forces are seen here and there inside the premises of the Hospital.
The entire Hospital, where a few medical professionals have returned through UNICEF’s mobile health and nutrition teams initiative, has been ransacked beyond recognition. An estimated 20 million Br worth of medicine and laboratory equipment went in a matter of weeks. A lone IV stand has been spared or forgotten.
Expired medicine, cigarette butts, syringes and shredded paper litter the floors of administrative offices, while spilled liquid solutions cover the walls of the examination rooms in colours of purple and red. The cabinets in more than one of these rooms contain faeces. With the Hospital's staff having fled due to the fighting, it had been an abandoned site until the recent arrival of the health workers.
The mobile team is one of 10 dispatched across the region’s eastern, central and northern fronts, equipped with limited and urgently needed medications such as insulin and antiretroviral therapy (ART) drugs to treat and suppress HIV. Nearly 40,000 people in the region are dependent on ART alone.
It has been three weeks since the team, made up of eight health workers, has been operating from a makeshift examination room in the Hospital. With no laboratory equipment and scant supplies, patients are treated based on a signs-and-symptoms diagnosis.
Even so, over two-thirds of the Hospital’s daily visitors are turned back for lack of necessary supplies, according to Alem Nirea (MD), the team’s medical doctor.
The team has been given two UNICEF-branded cars where they pack up the medicine and head out as night falls.
“We have no security here,” said Alem. “We're here because the community is suffering; they were happy to see us come.”
Hardly two weeks in and the team had already run out of the insulin and hypertension medicine they had brought with them.
Wuqro Hospital, though sustaining damage from shells during the conflict, has resumed activities at a 50pc operational capacity.
“A lot of people in the area have lost their lives, because they couldn’t get the medical care they needed,” said Alem.
Frewoini Hospital, established nearly two decades ago as a health centre, had slowly climbed its way to the status of primary hospital through material support from aid organisations and the region’s health bureau. It was serving an average of 150 people a day. Today, it has been forced to discontinue immunisation programmes, not unlike most of the region, with no refrigeration available for the storage of vaccines.
But it is not just the medicine and the equipment that has been stolen here. The Hospital’s entire electric wiring system has been torn out. Following the restoration of electric power in the area, it remains excluded from this small return to normalcy.
This has also meant that much-needed paperwork to trace the centre's day-to-day operations has been lost. A few weeks ago, a truck full of supplies ranging from basic requirements like beds to sterilising equipment worth 300,000 Br was sent to the Hospital from the regional office of the Ethiopian Pharmaceutical Supply Agency. It returned to the Agency’s office in Meqelle, unable to deliver the items for lack of a certain Model-19, a sign-over sheet.
The form, a template hospitals and health centres are required to provide in order to get their allotted medical equipment, is necessary for the Agency to audit its work. But like almost every other document in the Hospital, it has been lost among the debris. While the centres are currently operational during the day, full restoration has proven unrealistic in a region that is still largely insecure. For now, the teams are mobile, moving from one health centre to another and back to the regional capital before safety problems arise.
The latest assessment carried out by UNICEF reveals that equipment in over half of the 205 health facilities across the region is fully damaged or non-functional due to lack of supplies and staff.
The scene replicates itself from one health centre to the next along the road to the town of Frewoini. The Negash Health Centre, some 30Km closer to the regional capital, has been abandoned altogether after the looting. Its sprawling compound houses examination and registration rooms, floors thick with papers, gloves, and equipment dumped from their respective shelves. Here, there have been no efforts to rehabilitate. Some health centres have been luckier in this regard.
Headway has been made in Wuqro Hospital, which was shelled on November 24, 20 days after the Federal government launched an offensive against forces of the Tigray People’s Liberation Front (TPLF), the region’s now-ousted administration.
The order to attack came following an earlier pre-emptive strike by TPLF on the country's northern military base.
As the conflict slowly encroached from the outskirts of the Regional State and reached the town, the Hospital's staff had fled for cover, sending all critical patients to Meqelle with an ambulance, according to the Hospital’s Medical Director, Adonay Hans.
“We counted up to 120 shells in the first day the town was hit,” said Adonay.
Like many inhabitants of the town, he had spent 10 days seeking refuge in the caves located underneath the town’s mountainous surroundings.
The Hospital, though up to 50pc operational today, was also pillaged – laboratory equipment, AC machines from operating rooms, operating equipment and mattresses were all looted. Following a month-long closure, the Hospital’s staff had to be convinced to come back through a door-to-door call.
Security has since been doubled; and with a special permit from the mayor of the town, the Hospital has been granted a rifle to chase away any opportunistic thieves.
Sporadic shooting can be heard from time to time, according to residents in the nearby Gheralta mountains, a famous tourist destination well-known for its near-vertical hiking trails. Proximity to the capital has also ensured that Wuqro, which lies 48Km away from Meqelle, is more secure and, by extension, one of the few recipients of supplies from the Pharmaceutical Supply Agency.
Though the Agency provides equipment and medicine based on a needs report from facilities, it has been going off previous estimations, according to Hewan Semere, the Agency's regional deputy-manager.
Operational throughout most of the conflict, the Agency had come to a standstill at the end of November as the conflict progressed further into the city.
“By the time we'd restarted operations, most of the health centres were badly hit,” said Hewan. “We had no requests coming, so we were serving the ones near the capital.”
The Agency, which has two major sites of operation in the region at Meqelle and Shire, caters to over 300 government and privately-owned health centres but has only been able to reach 76 so far. Despite serving a fraction of its earlier demand, it is undergoing a severe shortage of medicine.
“The health centres all had stock for a few months ahead,” she said. “But since the looting, we've started from scratch, and that has created more pressure to supply these medicines.”
A lone example in the midst of all this has been Meqelle Hospital, which has continued providing its services through the conflict. This may be due to the fact that the military had not used it as a campsite, according to the Hospital’s Medical Director, Kahsay G. Medhin. Nearly 50 staff members left their posts at a certain point, but emergency care, maternity and vaccination services had continued, he explained.
Expecting mothers had lined up in its corridors and in adjacent hotels and guest houses; with no ambulance service and an imminent due date, they could not risk being too far from the Hospital. In the last month alone, there were over 700 deliveries at the Hospital, nearly triple the number prior to the conflict.
“We were using candles for most rooms and whatever fuel we had for the delivery and operation rooms at the time,” he explained.
Located in the centre of the city, the Hospital has now resumed activities, with 550 medical and non-medical staff back on duty. Widespread rape cases reported across the region have been registered here as well. It provides care for over 50 rape victims, most of whom came seeking abortion services – a last-minute resort for what would have otherwise gone unreported. Seven of the reported cases are underage girls.
But the government hospital faces a slightly different challenge than the rest. Its budget was cut from its annual 34 million Br to 26 million Br this year, and frozen bank accounts are causing operational problems.
The restoration of health centres, which took years to set up, has been initiated, but the continuation of essential health services, previously stretched thin following the Novel Coronavirus (COVID-19) pandemic, now faces an even bigger challenge in light of the conflict. Health professionals who advocate for basic services to be continued at any cost and under any circumstances warn of the longer-lasting effects that the interruption in immunisation programmes and the supply of medications for HIV, diabetes, tuberculosis, and others will have in the Regional State.
The strength of the region’s herd immunity, based on the prevalence of vaccinations given prior to the war, will largely determine how safe unvaccinated children are, explained Adamu Addissie (MD), assistant professor of public health at the College of Health Sciences at Addis Abeba University.
“Vaccinations for children can be given as soon as the services are re-instated,” he said. “Through finding out what has been missed, the child can receive all backlogged vaccinations.”
The approach for diabetes and HIV patients is more complex. Discontinuation may lead to resistance to medication for ART, possibly leading to AIDS, the late stage of the HIV infection where serious infections may lead to death.
This is to say nothing of the untold numbers who have already lost their lives.
PUBLISHED ON
Mar 13,2021 [ VOL
21 , NO
1089]

Radar | Apr 19,2025

Agenda | Apr 15,2023

Viewpoints | Apr 11,2020

Radar | Jan 31,2021

My Opinion | May 31,2020

Commentaries | Dec 26,2020

Covid-19 | Mar 21,2020

Fortune News | Jun 20,2020

Radar | Apr 24,2021

Radar | Jun 07,2020

Dec 22 , 2024 . By TIZITA SHEWAFERAW
Charged with transforming colossal state-owned enterprises into modern and competitiv...

Aug 18 , 2024 . By AKSAH ITALO
Although predictable Yonas Zerihun's job in the ride-hailing service is not immune to...

Jul 28 , 2024 . By TIZITA SHEWAFERAW
Unhabitual, perhaps too many, Samuel Gebreyohannes, 38, used to occasionally enjoy a couple of beers at breakfast. However, he recently swit...

Jul 13 , 2024 . By AKSAH ITALO
Investors who rely on tractors, trucks, and field vehicles for commuting, transporting commodities, and f...

Oct 4 , 2025
Eyob Tekalegn (PhD) had been in the Governor's chair for only weeks when, on Septembe...
Sep 27 , 2025
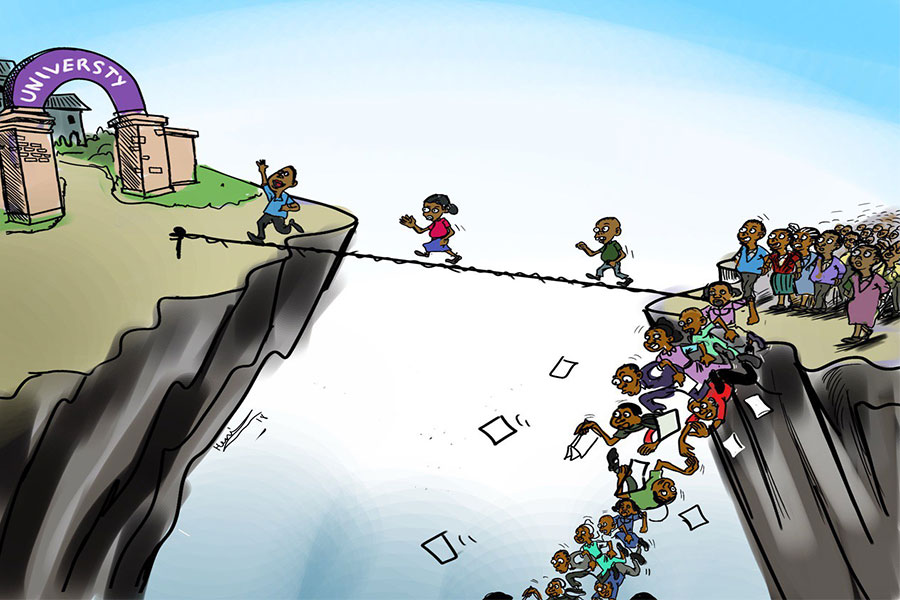
Four years into an experiment with “shock therapy” in education, the national moo...
Sep 20 , 2025
Getachew Reda's return to the national stage was always going to stir attention. Once...
Sep 13 , 2025
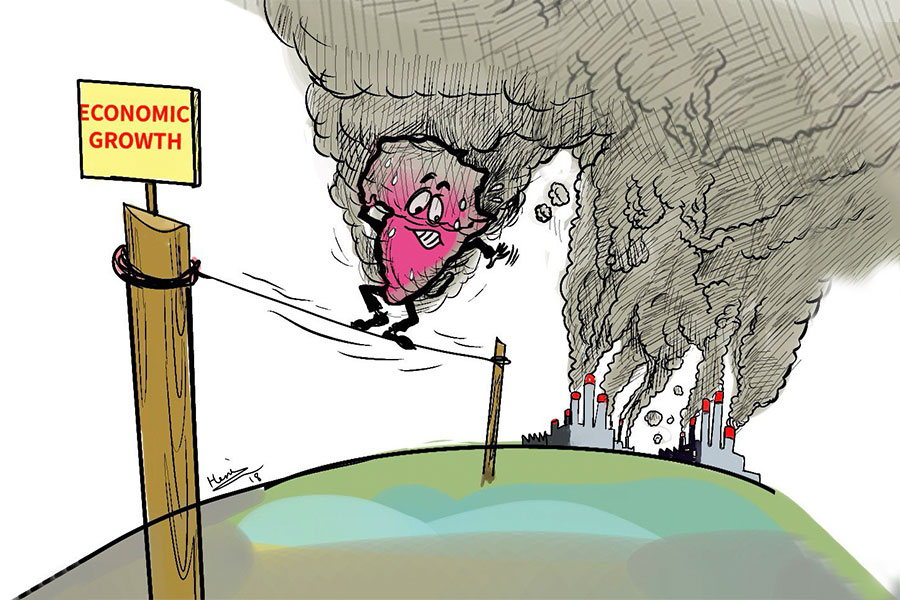
At its launch in Nairobi two years ago, the Africa Climate Summit was billed as the f...